You’ve been hearing, “Intestinal Permeability” quite a lot. But what exactly is permeability?
First, zonulin increases permeability.
So before we discuss permeability, let’s first review zonulin.
What is Zonulin?
Zonulin modulates intestinal permeability and is responsible for the intestinal and liver cells.
It governs the flow of fluid, macromolecules, and leukocytes between the circulation and the intestinal lumen.
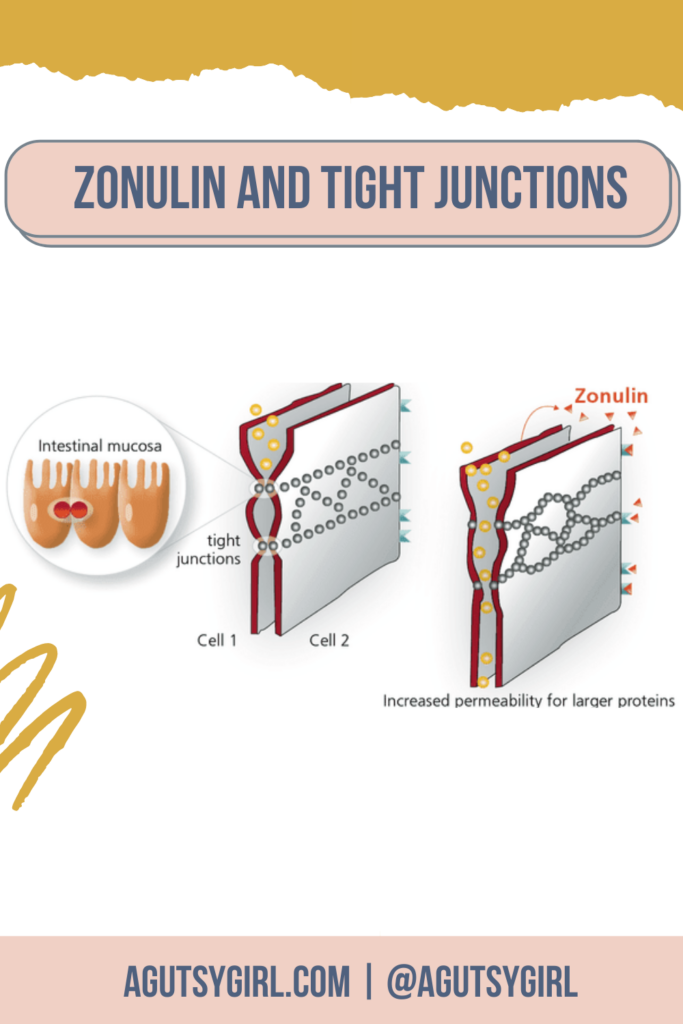
Tight Junctions
Zonulin is one of the markers for evaluating intestinal mucosa permeability.
Intestinal mucosa permeability is the degree of permeability of tight junctions between cells of the digestive tract wall zonulin maintains.
Epithelia and Epithelium
Epithelium is a word that refers to the inner and outer surface coating of the body.
It encompasses bodies, blood vessels, and cavities, including the skin.
The singular for epithelium is epithelia. There are tight junctions inside the epithelia of our bodies.
Zonulin and Leaky Gut
If you recall from my book, The Leaky Gut Meal Plan,” there is a strong connection between zonulin and leaky gut.
Tests for zonulin, IgG food intolerance, and vitamin and mineral deficiencies can help determine whether your gut is leaky, as can testing with lactulose.
In other words, testing zonulin levels is a leaky gut indicator.
Leaky gut and intestinal permeability are often interchanging words because of the process that occurs. A problem or ailment that occurs mainly within the small bowel lining is destroyed, causing “slips” through the intestines and the bloodstream to flood.
This process is also called “intestinal permeability.”
The undigested food particles, hazardous waste products that make bacteria leak in our body, are frequently the cause.
Permeability
So then let’s return to permeability.
Click HERE to save this post for later.
Permeability is the ability for electrolytes or molecules to flow through the pores of channel proteins. The power of substances to permeate the pores of channel proteins are critical.
When the permeability of capillaries is enhanced, proteins and other molecules are allowed to escape into the interstitial fluid. This results in inflammation.
The above description is a more complex way for describing my above commentary.
Function of the Gut
A single layer of cells that border your gut is called the mucosal barrier.
These cells are highly specialized, as they must enable the body to absorb all nutrients while also preventing harmful chemicals or invading infections from slipping through the mucosal barrier to bloodstream.
(Image credit HERE.)
Zonulin promotes intestinal permeability; the lining of the intestines can be thought of as a cheesecloth. It should only pass the smallest particles.
Zonulin makes the cheesecloth pores bigger and makes it possible for large particles to enter the blood and the body.
The “leaky” intestines process is hypothesized to lead to body-wide inflammation and potentially autoimmune disease development.
Remember, not everyone believes in “leaky gut.” I acknowledge that in my full post on What is Leaky Gut? HERE.
Factors that increase zonulin
In my book, I talk about gluten as a factor for increasing zonulin.
But here are two main factors for increasing zonulin:
Bacterial colonization
Bacteria that colonize our intestines are now universally recognized to have a substantial good and harmful effect on human health.
Several experiments have shown that certain bacterial species stimulate zonulin synthesis.
The increased expression of zonulin loosens tight connections and enhances intestinal permeability.
Gluten
According to an NPR article,
So what does it have to do with gluten? It turns out that gluten is a strong trigger of zonulin in some individuals. “No human being completely digests gluten,” says Fasano. “And in a small percentage of us, that undigested gluten triggers the release of zonulin,” leading to high levels of it.
Several studies have shown this gluten and permeability connection.
Zonulin Test
So the question you are asking right now, “Okay, so is there a way for me to test zonulin in order to understand more about my own gut health?”
As I mention in the beginning of this article via my book, yes, yes you can test zonulin levels.
Here are some zonulin testing sources for consideration:
- Go to your doctor, ask him/her about it, and proceed forward.
- Everlywell Food Sensitivity Comprehensive Test (code: AGUTSYGIRL at checkout will save you 20%)
- Gut Health Test by Thorne
- Zonulin Stool Test by Verisana
- Leaky Gut Complete Test by Verisana
- Food Inflammation Test (FIT Test) via KBMO Diagnostics
Food Inflammation Test (FIT Test)
According to KBMO Diagnostics,
The FIT Test is the most sensitive food test available using patented technology. The multiple pathway approach allows us to look at not only food sensitivities but also inflammation and gut permeability all from one test. We also provide best in class compliance tools including a personalized meal plan and a patient app.
Zonulin Test Uses
In the FIT test, Zonulin is one of three ways for diagnosing a leaky gut and detecting Candida sensitivity and a variety of food sensitivities, among other things.
Here are other conditions that have been associated with high concentrations of zonulin:
- Celiac Disease
- Autoimmune disease
- Multiple Sclerosis (in addition to other chronic illnesses)
Celiac disease
Increased zonulin levels free up tight bonds, and intestinal damage occurs for genetic predisposition (HLA-DQ2/8) and exposure to gluten.
Breaches of the intestinal barrier encourage pro-inflammatory signaling of T-cells.
The level of zonulin increases during the acute stage of the disease and decreases when removing gluten from the diet.
Serum zonulin was associated with permeability tests for lactulose/mannitol in celiac patients.
Non-celiac sensitivity to gluten (NCGS)
A 2015 study showed that those with NCGS have zonulin levels above the usual control group but below the values for those living with celiac disease.
IBD
Elevated zonulin levels are linked with the occurrence of atopic symptoms in children with IBD (Inflammatory Bowel Disease).
Diarrhea (Predominantly Irritable Bowel Syndrome (IBS-D)
Again, a 2015 study showed that individuals with zonulin levels above normal control populations but below coeliac disease levels.
The HLA-DQ2/8 genotype is related to increased transit times in this population.
Type 1 Diabetes (T1D)
It is still necessary to clarify the autoimmune source of pancreatic β-cell disorder.
Nevertheless, 40% of Caucasian people who have T1D have a genetic predisposition (human antigen leukocyte (HL-A) alleles), resulting in the emergence of the disease in combination with environmental causes.
In human and animal research, exposure to gliadin is associated with the expression of T1D.
Recent investigations show that gastrointestinal signs are linked to increased intestinal and zonulin permeabilities in T1D patients before GI problems occur.
Human experiments have demonstrated that non-diabetic relatives of the family (with identical heritage) have frequently elevated zonulin and intestinal permeability.
Liver disease
Obese and nonalcoholic fatty liver disease in teens and young people showed greater zonulin levels than their age, sex, and similar BMI controls.
Multiple Sclerosis (MS)
All of the diseases were more common in MS patients, except excessive cholesterol.
They had high rates of mental illness, notably depression. According to the study, 19% of MS patients and 9% of those without MS suffer from depression.
There were considerable gender differences in many of the chronic diseases.
High blood pressure was reported by 22% of males with MS and 15% of men without MS, compared to 14% of women with MS and 12% without MS.
Studies show that near asymptomatic relatives can commonly have higher zonulin and intestinal permeability in many conditions associated with increased intestinal permeability, such as Crohn’s disease.
Most develop their symptoms in a few years.
Doctor’s Data
In 2014 I did a comprehensive stool test via Doctor’s Data.
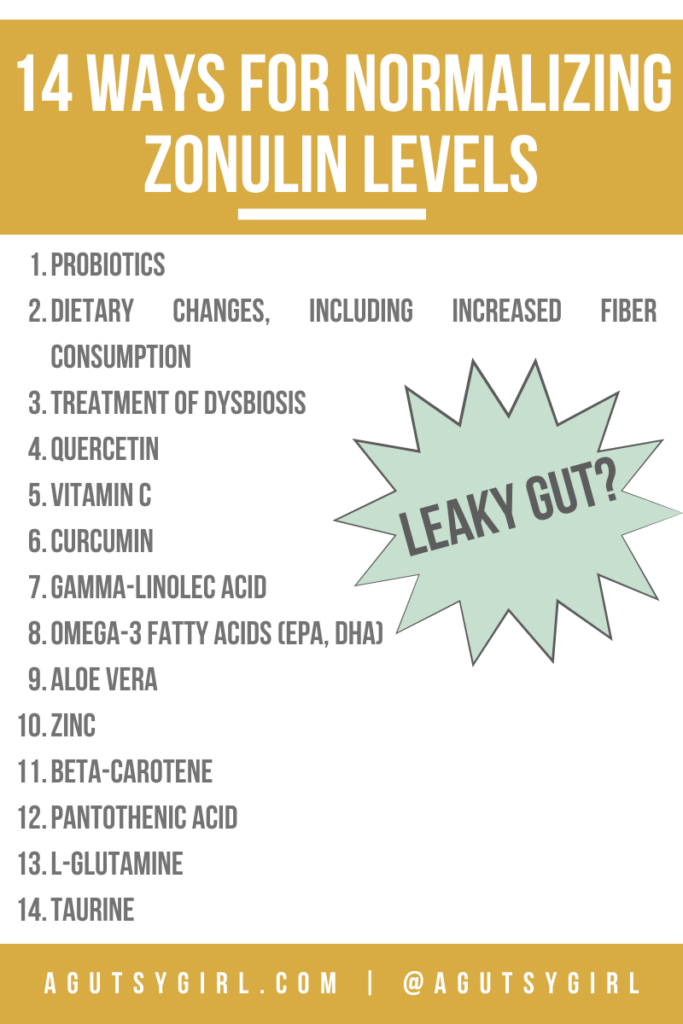
Doctor’s Data is also on the cutting edge for zonulin information. In a large article they produced on zonulin, they provide many ways for normalizing zonulin levels.
According to the article, here they are:
- Probiotics (I choose the Just Thrive Probiotic, and HERE is why as it relates to Leaky Gut Syndrome)
- Dietary changes, including increased fiber consumption
- Treatment of dysbiosis
- Quercetin
- Vitamin C
- Curcumin
- Gamma-linolec acid
- Omega-3 fatty acids (EPA, DHA)
- Aloe Vera
- Zinc
- Beta-carotene
- Pantothenic acid
- L-glutamine
- Taurine
Sources: HERE, HERE, and HERE.
If you’re struggling and seemingly reacting to everything, read through this post again. Then, grab one of my food and lifestyle journals. And, of course, consider any and all testing.
If you liked this post, you might also enjoy:
- Beef Bone Broth Recipe for Leaky Gut
- How Long Does it Take to Heal Leaky Gut {Troubleshooting the Diet}
- The Leaky Gut Meal Plan is Not a Diet
Xox,
SKH
🤰 bloating be gone! weight loss through optimal gut health for women
💃ʜᴇᴀʟ ʏᴏᴜʀ ɢᴜᴛ. ʜᴇᴀʟ ʏᴏᴜʀ ʟɪfe.
🫶🏻 founder gutbyome.com