What is the difference between probiotics vs antibiotics, what are the side effects of antibiotics, and how can you rebuild the gut lining after antibiotic use?
Probiotics vs Antibiotics (Side Effects of Antibiotics and Rebuilding the Gut) (Episode 102, Bites #37)
Click HERE to save probiotics vs antibiotics for later.
Episode 102: Show notes
Episode 102 on the ‘A Gutsy Girl‘ podcast: Probiotics vs Antibiotics (Side Effects of Antibiotics and Rebuilding the Gut) (Episode 102, Bites #37) Get my 9 strategies for post-antibiotic use to ensure a healthy gut microbiome.
In this Episode we cover:
- What are antibiotics?
- Side effects of antibiotics
- 9 specific strategies for repairing the gut after a course of antibiotics
Links & Resources Mentioned in this Episode:
- The probiotic we use and love in our family = Just Thrive Health (code AGUTSYGIRL will save you 15% at checkout)
- Dissecting Dysbiocide
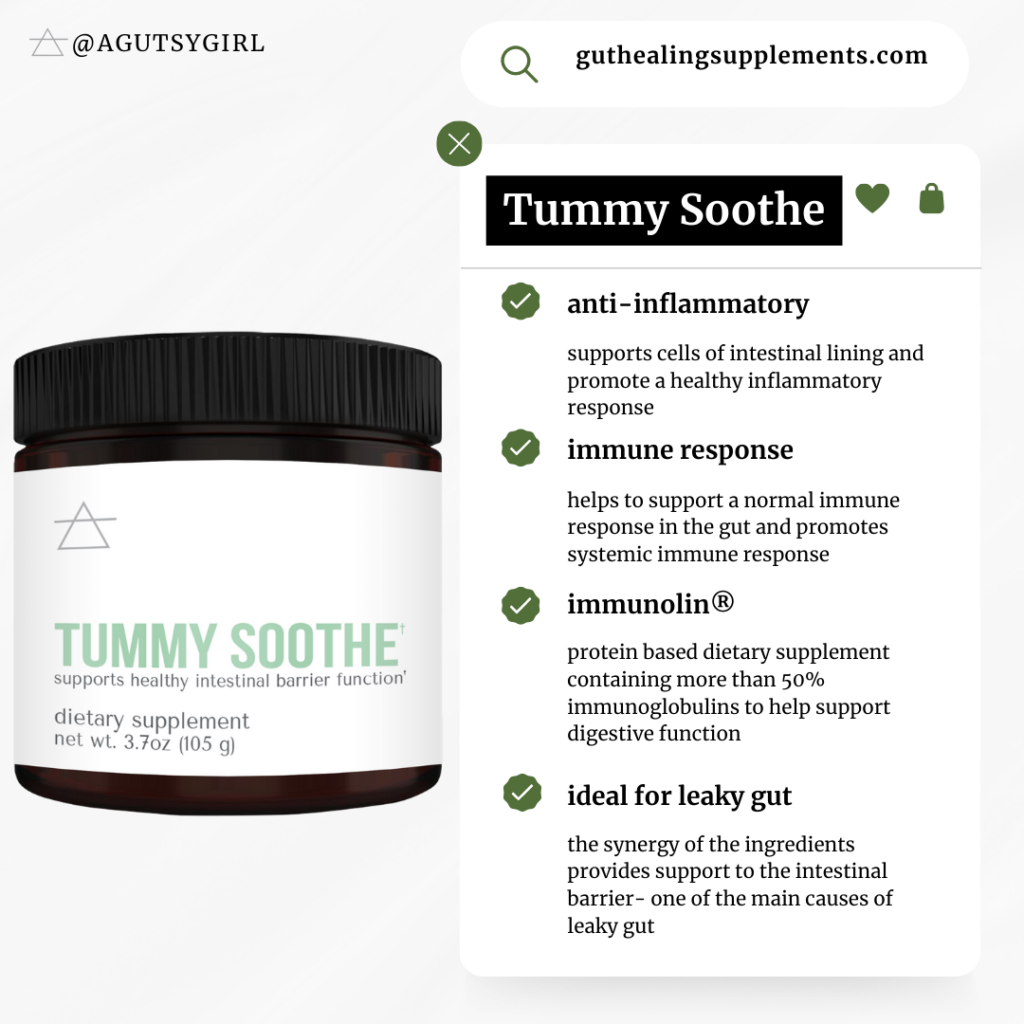
- Tummy Soothe (code PODCAST at checkout to save 15%)
- Fasting to Cure SIBO {thoughts on Intermittent Fasting for SIBO} {Episode 53, AGG Bites #8}
- 192 Sources and Alternate Names for Sugar
- 15 Supplements for Stomach Lining Support
- Re-Build – top-quality collagen (code PODCAST at checkout to save 15%)
- Reasonable SIBO
- A Gutsy Girl’s Bible: a 21- day approach to healing the gut
- The First Three (a free 3-day gut reset)
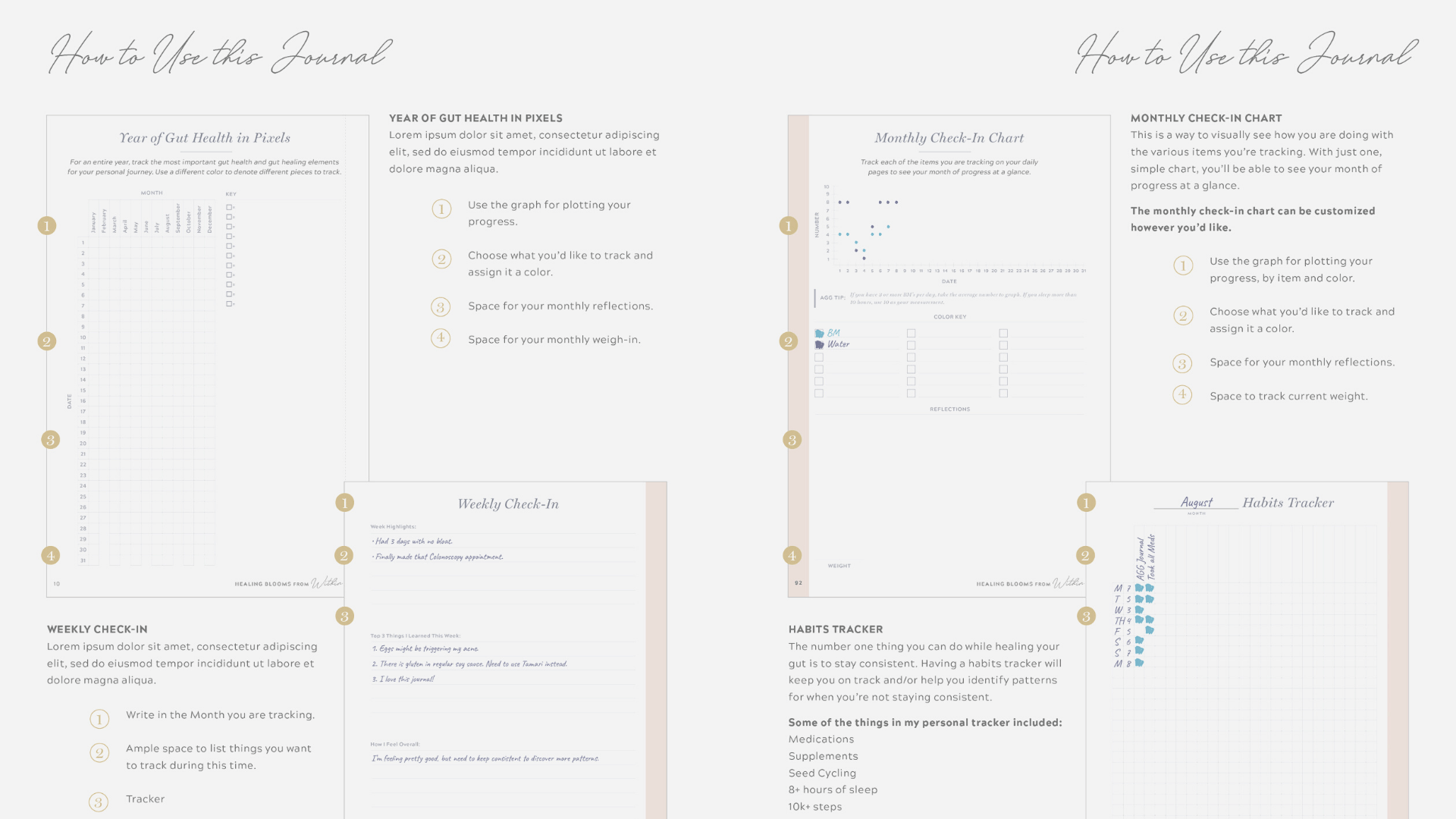
- Your gut healing journaling system
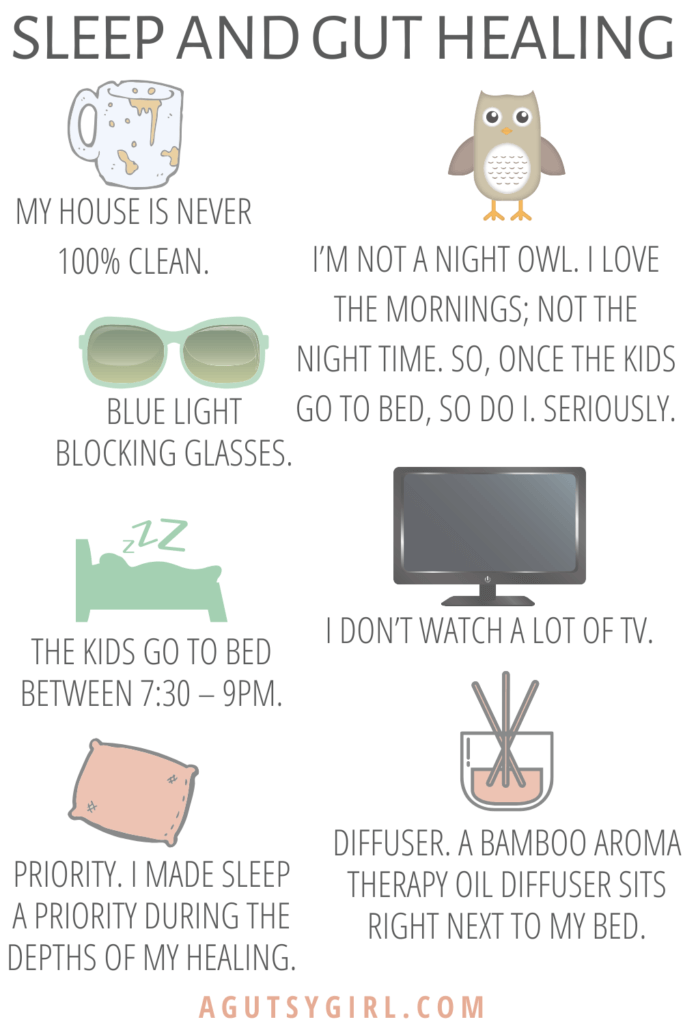
- Sleep and Gut Healing
Episode Images
More about the A Gutsy Girl Podcast
A Gutsy Girl is the podcast that teaches, preaches, and celebrates healing the gut and living a happier, healthier life.
More episodes you might enjoy:
- Welcome to A Gutsy Girl Podcast
- Hang out on Instagram
- BFF’s on YouTube
- Free resource: The Master Gutsy Spreadsheet
- Rated-G Email Club
Side Effects of Antibiotics and Rebuilding the Gut
Click HERE to save this post on probiotics vs antibiotics + rebuilding the gut for later.
I am constantly being asked two things as they relate to probiotics vs antibiotics:
- Is it okay if I have to take an antibiotic course? and
- How can I keep my tummy happy during and after antibiotics?
So let’s dig in, mmmmmkay?
What are Antibiotics?
Let me break this down as simply as I can to start the discussion.
The National Library of Medicine states that antibiotics are,
powerful medicines that fight bacterial infections. Used properly, antibiotics can save lives. They either kill bacteria or keep them from reproducing. Your body’s natural defenses can usually take it from there.
- Anti = opposed to, against
- Pro = for, beneficial
Antibiotics, while they can be life saving, can disrupt the natural gut microbiome, leading to various digestive issues and potential susceptibility to infections.
One of the main issues with antibiotics is that, as a whole, we have become resistant to them.
And the overuse of antibiotics is clearly driving the evolution of resistance.”
Antibiotics work for bacterial, not viral, infections.
Some of these viruses include:
- Colds
- Flu
- Most coughs and bronchitis
- Sore throats, unless caused by strep
If a virus is making you sick, taking antibiotics may do more harm than good.
Using antibiotics when you don’t need them, or not using them properly, can add to antibiotic resistance. This happens when bacteria change and become able to resist the effects of an antibiotic.
The Problem with Antibiotics
Antibiotics, as originally intended, can be life saving. There is no denying that, though many will try to argue it.
The modern era of antibiotics started with the discovery of penicillin by Sir Alexander Fleming in 1928. Since then, antibiotics have transformed modern medicine and saved millions of lives. Antibiotics were first prescribed to treat serious infections in the 1940s. Penicillin was successful in controlling bacterial infections among World War II soldiers. source
Problems began after that, when resistance developed with Penicillin and then eventually, with other antibiotics as well
Side Effects of Antibiotics
But let’s say that you have a bacterial infection and need the antibiotic. Then what? Is it okay to take them?
YES! Listen, I learned my lesson the hard way in April of 2014. I wrote about it via Antibiotics (<- go check out the post).
Seriously, friends, we must stop antibiotic-shaming. If you are living your life proactively vs. reactively 90% of the time, then the other 10% you need to react.
You have a choice here, as always, but I trust that you’ll make the right one. More important than that, though, is that you will do so without shame.
But yes, it’s true, there is a plus/minus to everything in life. Antibiotics are no different.
Rebuilding the gut after a course of antibiotics is essential to restore the balance of beneficial bacteria and support overall gut health.
Here are some common side effects of antibiotics:
- Stomach problems (including the risk of antibiotic-associated diarrhea), nausea and vomiting.
- Thrush infections, which can affect the mouth (white patches will be visible) and in women can also occur in the vagina (causing itchiness, pain and discharge).
- Ongoing diarrhea caused by an intestinal infection, which may be serious and require further investigation and treatment.
- Allergic reactions, such as hives (large, red, raised areas on the skin), fever and breathing problems.
- Bodily infections resistant to antibiotics.
- Swollen, black, or “hairy” tongue.
- Menstrual cycle problems.
- Hallucinations, psychotic reactions and tendon ruptures.
(Keep in mind that different antibiotics have different side effects, and that this is not an exhaustive list.)
Rebuilding the Gut After Antibiotics
Listen, I love and respect all the natural, integrative, and functional doctors / doctors with websites out there. I study and learn alongside them, and I will always be on their side.
That said, sometimes I feel like we can get too wrapped up in every last thing they say about the negatives on Western medicine.
I believe there must be a better balance because as it stands today people are typically using too much or too little medication; I’ve found problems with both.
Hear me clearly on this: sometimes you just need the damn medication.
Today, what I want you to know is this fact, “After antibiotic treatment, our gut microbiota usually recovers to its previous state a few weeks or months later.”
If it’s a good idea that you take an antibiotic, take it. Focus on it, don’t let the guilt weigh you down (because that will do your system even more damage), and then move on.
The good news is that there ARE ways to easily move forward after any antibiotic therapy needed.
9 Simple and Practical Ways for Rebuilding the Gut After Antibiotics
Click HERE to save these ways for later.
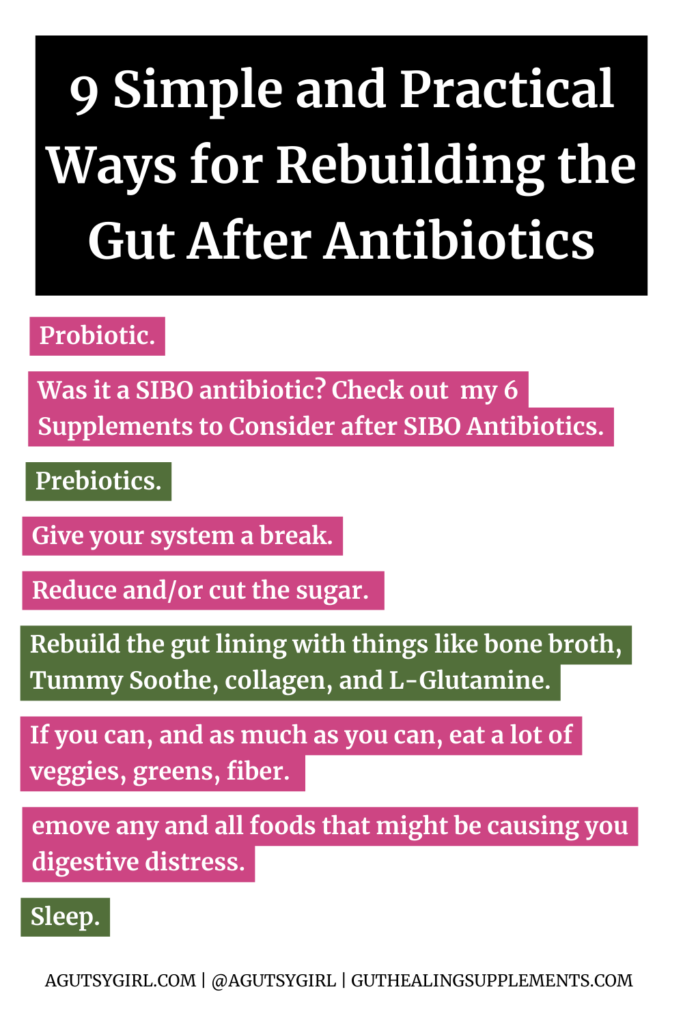
1. Take the probiotic
You might have heard of a probiotic before because it seems like everyone is talking about probiotic supplementation.
Probiotics vs antibiotics sound similar, but definitely are not. Their affects on the digestive tract are very different.
A probiotic stimulates the growth of beneficial bacteria whereas an antibiotic is intended to treat bacterial infections and diseases with the intention of killing bacteria.
Think of it this way — one helps build the army and the other destroys it.
The benefits of probiotics range from aiding in the reduction of gastrointestinal symptoms to the reduction of skin issues like Atopic dermatitis and have even proven to have mental health benefits.
But probably the number 1 question I’m asked is,
What probiotic do you recommend?
Let me first make it clear that this is a difficult question to answer, as the type of probiotic supplements that are beneficial for one person might be different for another.
The use of probiotics is individualized, similar to your overall gut-healing journey, and there are so many probiotic products on the market.
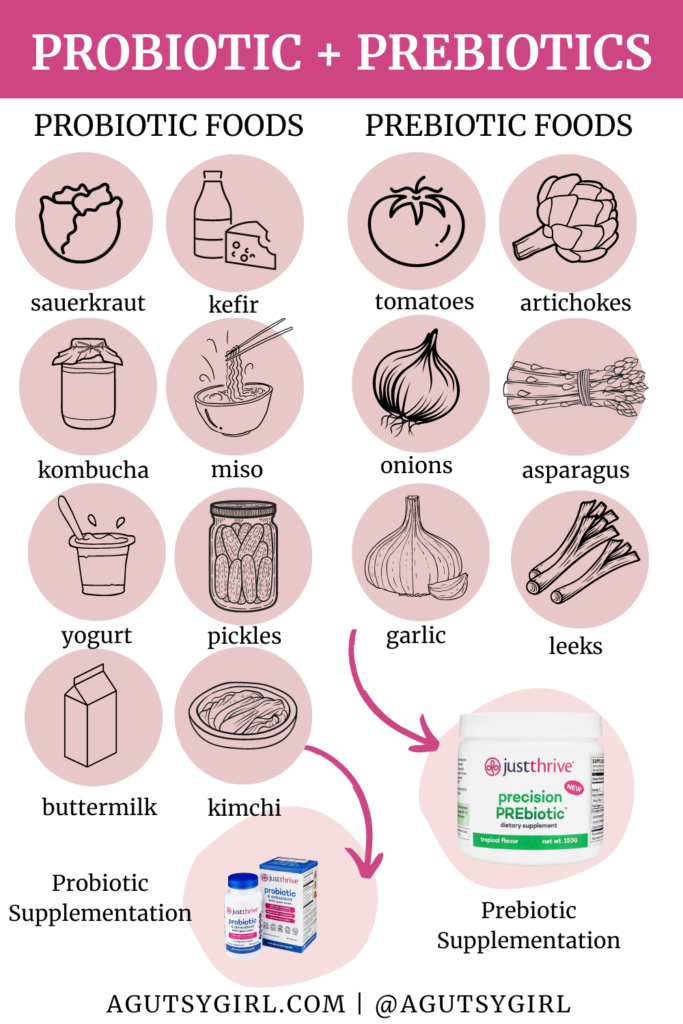
Now, There are two main ways we get probiotics; via probiotic supplement and/or by consuming probiotic-rich foods.
Probiotic foods include:
- Yogurt naturally contains probiotics, but some manufacturers add additional strains, such as L. acidophilus
- Miso is a fermented soy-based condiment. It makes an awesome flavor addition to soup
- Fermented vegetables, such as sauerkraut, pickles and kimchi, especially those that are homemade or sold refrigerated
- Kombucha is fermented tea
- Kefir is a fermented thick drink, similar to yogurt, but made by inoculating cow, sheep or or goat milk with kefir grain
- Buttermilk is fermented milk. Traditionally, it was made from the liquid left behind after churning butter, but most modern buttermilk is cultured
- Creme fraiche is a thick dairy product, similar to sour cream
The other way to get more probiotics is by taking a probiotic supplement which in and of itself has many health benefits.
Probiotic Treatment via Supplementation
When looking at a probiotic label, you will either see two or three words that describe the type of probiotic.
These two or three words include some or all of the following: genus, species and probiotic strains.
- An example of two: Lactobacillus (genus) acidophilus (species)
- An example of three: Bacillus (genus) subtilis (species) HU58 (strain)
When you see two words, that means the manufacturer has listed only the species, not the strain, of probiotic being used. And when you see three words, such as Bacillus subtilis HU58, the manufacturer has listed the specific strain of probiotic used.
You can learn more about strains of probiotic bacteria HERE.
But to answer the question directly, I personally use, as does my whole family, Just Thrive Health probiotics.
I have an entire episode all about this probiotic that you might want to check out — Episode 9, Gut Definition.
AND because i exclusively use them, you can always use my code AGUTSYGIRL at justthrivehealth.com to save 15%.

Now you can get this probiotic in gummies form, if desired.
2. Was it a SIBO antibiotic?
I wanted to be sure to add this one in here as there are so many with diagnosed SIBO now who are going the antibiotic route. I did, too. And that’s how I know so much about it.
One thing to make note of as it relates to the type of medication that the SIBO antibiotic is that the SIBO antibiotic stays localized to the small intestine (which is a good thing). i.e. Rifaximin is a nonsystemic antibiotic, which means that the drug will not pass the gastrointestinal wall into the circulation as is common for other types of orally administered antibiotics.
And what this means ultimately is that many people will not have the same potential adverse effects that many other antibiotics create.
Anyways, here are 2 clutch supplements to consider after a course of SIBO antibiotics:
- Dysbiocide: According to my doctor, a lot of people take this as “maintenance” for post-SIBO antibiotics to help ensure SIBO keeps at bay. It supports gut healing, microbiome health, and the immune system. He told me if I’m feeling perfect to not take it, but if I even feel a little off, to take it for one week, then have three weeks off. Rinse and repeat as needed. I have zero affiliation with the company; just love the product.
- Tummy Soothe: this is from my own supplement line, and I swear by it as a clutch product for overall immune response! Episode 105 is all about this supplement and why I believe almost everyone could benefit by taking it daily. But essentially, Tummy Soothe contains Immunolin which is an antibody. Think of it like the “bouncer” of your immune system. Its job is to bind to and remove things that are not supposed to be in your system. And in the episode, my guest specifically said that those who take antibiotics will benefit from it. I cannot stress this one enough, and you can learn all about it at guthealingsupplements.com. You can also use code PODCAST at checkout to save 15% if you want to try it.
Helps to support a normal immune response in the gut and promotes systemic immune response.
3. Eat prebiotics freely, responsibly.
Prebiotics feed the good gut flora to help more flourish.
Simply put, prebiotics are fiber-rich foods that feed the bacteria in your gut to promote even more healthy bacteria. Prebiotics are created from other bacteria your body has already created.
They benefit good bacteria exclusively by:
- They can lower the pH of the intestines by feeding the bacteria that produces lactic acid. The low pH wards off pathogens, which tends to grow in higher pH environments.
- When the levels of good bacteria grow, they produce antibacterial molecules that ward off bad bacteria.
And here’s the thing — probiotics cannot survive without food, which is where prebiotics come in. In other words, probiotic use is not as beneficial without the use of prebiotics as well.
Think of prebiotics as the plants and prebiotics as the fertilizer.
Three things to know about prebiotics:
- They are not absorbed in your upper gastrointestinal tract
- Prebiotics resist the acidity of the stomach
- They have the ability to be fermented by intestinal bacteria
Prebiotics are the fibers that your body can’t digest, but that the gut loves.
Here is a great graphic on probiotics vs prebiotics and how get them both into your everyday life.
4. Give your system a break.
Now, this one might come as no surprise, but I have to mention it.
If you were taking an antibiotic, then that means your body was already under stress due to the illness. Add the antibiotics and anything else you did to get well only added to that stress and inherent “work” the digestive system had to endure.
Therefore, one thing I always do after a course of antibiotics is let my digestive system rest.
And I do this by both intermittent fasting plus meal spacing religiously for a few weeks.
I am not saying do not eat. In fact, that could not be further from the truth. You NEED to repair and replenish now more than ever, but instead what I’m saying is to properly time out eating patterns.
Intermittent Fasting is simply the time from when you eat your last meal of the day until the time when you consume your first meal the next day. And meal spacing is the amount of time between each meal during the day.
At Cedars-Sinai, they, studied healthy humans to look at the gut microbiome to see how it changes with 2 fasts per week.” And here is what they found,
At the 12-16 hour mark, we saw a dramatic shift in the gut microbiome population after fasting for that period. Certain bacteria are super responsive to fasting, and those tend to be beneficial bacteria. The concept is that with intermittent fasting, you could permanently grow those bacteria and experience the associated benefits.
I have a whole podcast episode on this topic and the beneficial effects both intermittent fasting and meal speaking provide via Episode 53, Bites #8 that you can listen to HERE.
In the episode I break down both intermittent fasting and meal spacing and also share with you exactly how I approach them both on a daily basis.
5. Reduce and/or cut the sugar.
While I believe this is a practice we should be doing no matter if we took an antibiotic or not, I also believe that during any bout of illness and after antibiotics we must be even more cognizant of it.
Why?
Because sugar loves to feed bacteria, and remember the goal of an antibiotic is to get rid of unwanted bacteria. Side note: sugar does not discriminate between good and unwanted bacteria. It’s just there to feed any and all of it.
This one is NOT easy. Believe me, I know.
And yet, this is a health hack that healthy people practice daily.
But as best you can, reduce and/or cut the sugar for best long term results post-antibiotics.
6. Rebuild the gut lining.
Antibiotics set out to destroy.
So, now that they have done their job, your job is to rebuild.
My FAVORITE ways to rebuild the gut lining are with:
- Bone broth
- Tummy Soothe
- Collagen – ours from guthealingsupplements.com was very intentionally named RE-BUILD for this purpose and
- L-Glutamine. Spoiler alert – keep your eyes peeled because we are launching our own pure L-Glutamine called Gut Support in the coming days.
In fact, I have a whole article called 15 supplements for stomach lining support that you can review if desired, but if I had to choose a few super easy ways to get started these would be it.
If you want a pro tip and hack, here is exactly how I approach all 4 that I just mentioned:
- Step 1: I make homemade bone broth – or buy super high-quality packaged bone broth like one from Kettle & Fire.
- Step 2: Make sure the broth is heated and hot and add in a scoop of Tummy Soothe – stir until dissolved. Then
- Step 3: add in a scoop of collagen – stir until dissolved. And finally….
- Step 4: add in a scoop of L-glutamine, stirring until dissolved.
I do this at least once, if not 2-3 times per day after antibiotics.
7. Veggies, greens, and fiber.
And speaking of rebuilding the gut lining – now is the time to choose veggies, green and other high fiber foods.
If you can, and as much as you can, eat a lot of veggies, greens, fiber. (I realize this isn’t practical for all of you, but if you’ve ever read my guide called Reasonable SIBO there is a way that you can eat these things without feeling miserable.)
The reason for doing this is that these foods will help create bulk to the stool, flush through your system while also providing help for creating good gut bacteria.
Also, they will provide many great nutrients you might have missed out on while you were sick.
133-page guide on everything I did to heal my SIBO for good.
8. Remove foods causing you distress.
And to that extent, the next one is to remove foods causing you distress.
I know what you’re thinking right now — but what are these foods and how determine what this looks like for me?
If you have no idea, there are three best places you an start today to understand more:
- If you want a quick freebie – grab my FIRST THREE 3-day email series. This will guide you through the first three days AND you’ll also get, for free, the YES to and NO to food lists from my book, A Gutsy Girl’s Bible: a 21-day approach to healing the gut.
- And if you want the full run down with the lists, instruction, and food ideas, then just grab the whole book, A Gutsy Girl’s Bible.
- Finally, get my gut healing journaling system so you can track for yourself – it’s, hand down, the best way to know which foods are truly causing YOU distress.
Regardless, you’ll want to make sure you’re avoiding the foods that don’t work for you because remember, food is medicine. And right now, you want the best medicine for you and to avoid the foods that possibly contributed to illness in the first place.
9. Sleep
And last, but certainly not least — SLEEP.
Sleep, yes good old sleep is seriously one of the very best things you can do during and after illness.
It’s great for healing the gut and healing your life.
Antibioticos
I really hope this helped you not only understand probiotics vs antibiotics in greater detail, but also to help erase the antibiotic fear-state we are currently living in.
Do everything you need to to avoid having to take a dose of antibiotics in the first place, but when you do need them, “give in,” get better and continue healing your gut.
Work with your healthcare provider for even more strategies during and after the use of antibiotics.
Questions regarding probiotics vs antibiotics? Or anything else? Ask away.
If you liked this article on probiotics vs antibiotics, you might also enjoy:
Xox,
SKH
🤰 bloating be gone! weight loss through optimal gut health for women
💃ʜᴇᴀʟ ʏᴏᴜʀ ɢᴜᴛ. ʜᴇᴀʟ ʏᴏᴜʀ ʟɪfe.
🫶🏻 founder gutbyome.com





I love this! It does seem like if I take antiobiotics it will take away from healing, but they are a wonderful thing for some issues. No more shame in the antibiotic game!
Great timing! I just finished a round of antibiotics for H. Pylori.
Hi! Thanks so much for all of this wonderful info. You are truly a resource. I just finished a round of rifaximin and a few days later I got strep! Teacher life! I’m on low fodmap so not many prebiotics going on. I’m afraid that the amoxicillin is going to undo any repair the rifaximin did. Any thoughts? Thanks!!
Hi Bryanna – thank YOU for joining the journey with me. Don’t be afraid. Here is a great resource to help –> http://bit.ly/aggseanti
Hello sarah!
I have been prescribed doxycycline for a tick bite. I’m afraid to take it due to all the research saying that taking antibiotics can kill all good bacteria in your stomach and leave the bad (I already have sibo and I’m worried it’ll get worse). What can I do after this round of antibiotics to ensure this doesn’t happen? They say to take a probiotic midday when you take antibiotic doses morning and night for the 14 day period. But won’t that just kill them?
Take the probiotic if that’s what was recommended. Typically doctor’s recommend that to offset some of the negative effects of the antibiotic. Good luck!