What are some home remedies for Colitis? Today I have 21 to share.
What is Colitis?
Colitis, specifically ulcerative colitis, is an inflammatory condition classified as such:
a chronic (ongoing) disease of the colon, or large intestine. The disease is marked by inflammation and ulceration of the colon mucosa, or innermost lining. Tiny open sores, or ulcers, form on the surface of the lining, where they bleed and produce pus and mucus.
According to the Crohn’s & Colitis Foundation of America,
Colitis is marked by an abnormal response by the body’s immune system. The immune system is composed of various cells and proteins. Normally, these protect the body from infection. In people with IBD, however, the immune system reacts inappropriately. Mistaking food, bacteria, and other materials in the intestine for foreign or invading substances, it launches an attack. In the process, the body sends white blood cells into the lining of the intestines, where they produce chronic inflammation. These cells then generate harmful products that ultimately lead to ulcerations and bowel injury. When this happens, the patient experiences the symptoms of IBD.
UC symptoms can include: abdominal pain, blood in stool (bloody diarrhea), change in bowels, constipation, fever, weight loss, fatigue and more.
Colitis is a type of inflammatory bowel disease which is classified as many different things, and depending on what classification you fall under, your symptoms of ulcerative colitis likely vary.
This is the reason why people think when I say I have colitis it’s the typical colitis….it’s typically not what they think. I have proctitis, but there is also: proctosigmoiditis, left-sided colitis, pancolitis and fulminant colitis.
What ulcerative colitis is not is irritable bowel syndrome (though many people with ulcerative colitis symptoms also present with IBS symptoms).
It’s very important to understand the differences between IBS vs IBD.
IBD Patients Flares
It seems like so long ago since I had a Colitis flare up, but even still, I remember crystal clear what they were like and what I did while going through them.
I wrote about it via Food & 3 Things to do During a Colitis Flare Up. I have also written Learn to Cook: Top 10 Tips for Cooking with Colitis.
Both posts provide some helpful information, but I have learned so much about gut healing during my journey, and while I still agree (mostly) with my thoughts before on “what to do during a Colitis flare up,” I also believe that I would be doing you no favors if I didn’t tell you what I believe is likely even more important than my former suggestions.
In case you don’t want to go back and read the former posts, I will add pieces of them to this one for your convenience.
[Millions of women sit in pain, in silence, day-in, day-out. I know because I used to be one prior to my “Gutsy Girl” days. This is my contribution to all of you out there, and if you know women in your lives who are struggling, click HERE to share this on Facebook, with the hopes that they might see it!}
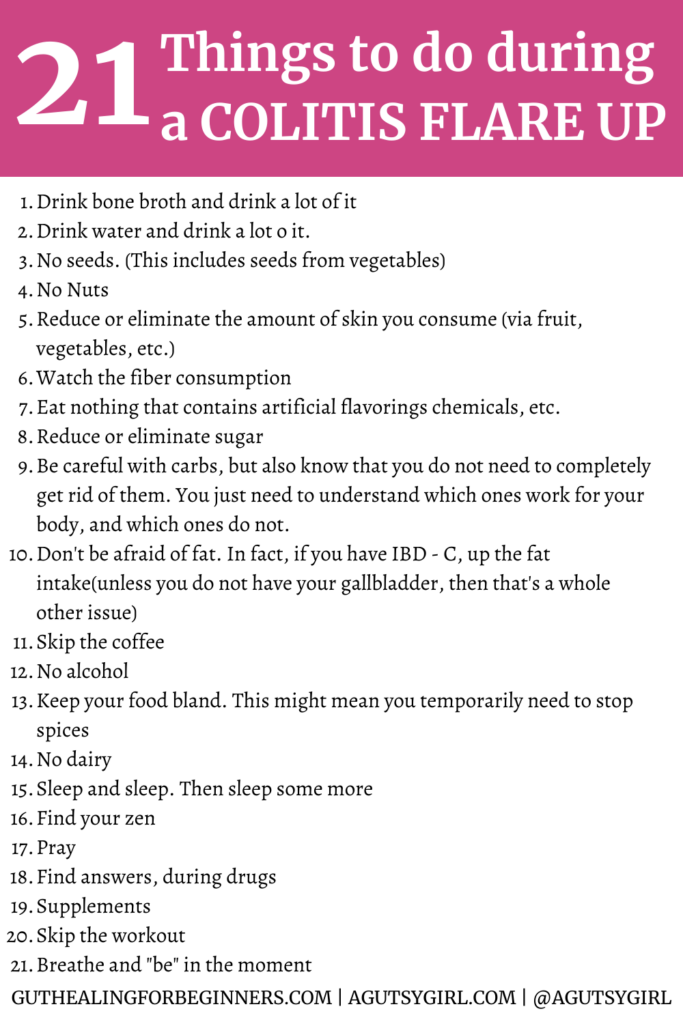
Home Remedies for Colitis (21 Things to Do During a Colitis Flare Up)
Click HERE to save these home remedies for colitis + 21 things to do during a Colitis flare up for later.
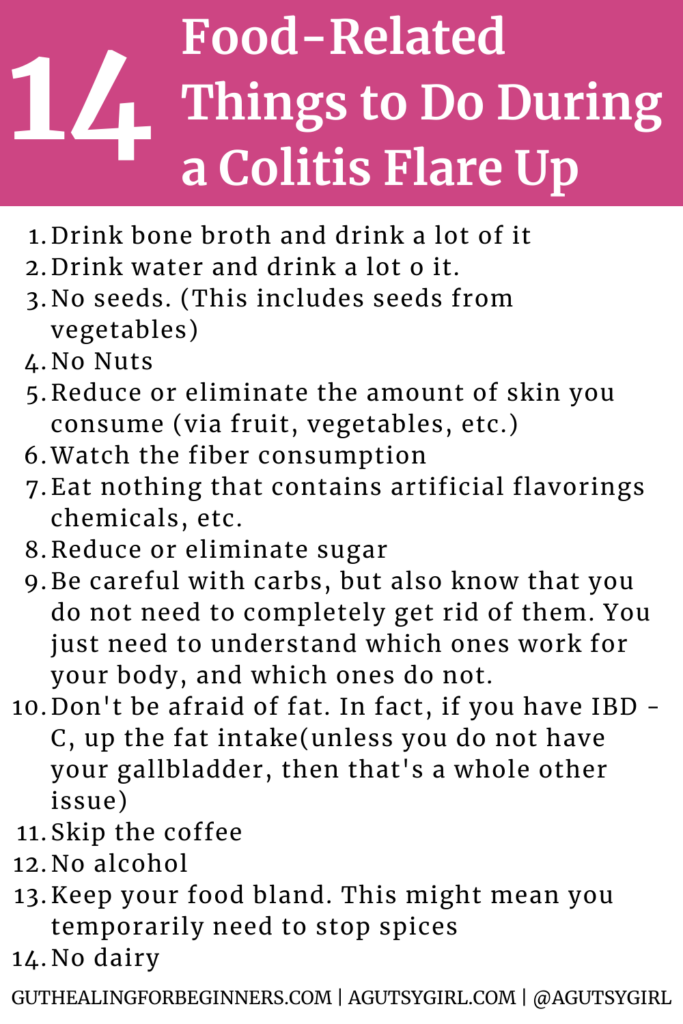
14 Food Related Things To Do During a Colitis Flare Up
Click HERE to save these 14 home remedies for colitis – food related – for later.
While mainstream medical likes to pretend that a healthy diet doesn’t matter for the treatment of UC, I beg you to consider otherwise.
At the very least, think about this: how could dietary changes not make a difference when UC is a chronic condition which lies within the digestive tract? Telling people that food doesn’t matter for the gastrointestinal tract is like telling us oil doesn’t matter for your car.
So I’m starting with 14 food-related things to try during a Colitis flare up.
Bone Broth
Drink bone broth, and drink a lot of it.
Side note: If making broth is never going to be in your future, but you are looking to still reap the benefits, choose THIS packaged bone broth. (Alternatively, drink vegetable broth, although I do not personally think it provides nearly the same benefits.)
There is an old South American Proverb which states,
Good broth will resurrect the dead.
And here are the bone broth health benefits as they relate directly to your GI tract and inflammatory response:
- Rich in gelatin. And I believe in gelatin for gut healing.
- Immune system boost. Because bone broth is packed with proteins (glycine and proline) that are well-known for nourishing the lining of your gut, it is thought to help give your immune system a boost.
- Nutrient dense. Bone broths contain minerals in forms that your body can easily absorb: calcium, magnesium, phosphorus, silicon, sulphur and others.
- Helps Leaky Gut Syndrome. You can read all about it in 31 Specific Things to Heal a Leaky Gut.
- Improve joints. Bone broth is a natural source of collagen, which is great for the joints and alleviating joint pain.

Easy access to the best-tasting + high-quality packaged bone broth.
Use code ‘AGUTSYGIRL’ at checkout to save 20%.
Water
Drink water, and drink a lot of it. (Don’t like it? Me, neither. Try this instead.)
Water is so often overlooked. It’s not just good for gut health, but overall health and we need it every single day.
Especially while in a Colitis flare, it’s a good idea to drink more water.
No seeds
While I believe in seeds and nuts for overall health, I also think that seeds while flaring won’t do you any favors.
This includes seeds from vegetables and also things like psyllium seeds. And when I was flaring, I simply just cut them altogether.
No nuts
Similar to seeds, I also cut all nuts during any flare state.
Skins
Reduce or eliminate amount of skins you consume (via fruit, vegetables, etc.).
The goal of getting through a flare is to consume specific foods that are easy to digest. Seeds, nuts, skin, and fibers are not easy to digest.
Fiber caution
Watch the fiber consumption. Read: Is Fiber Helping or Hurting Me?
Now, I’m ALL about fiber for optimal gut microbiome health, so cutting fiber is NOT a long-term treatment by any means.
And during periods of remission I believe you must figure out a way to get more fiber, whatever and however that might look for you personally.
But for today, go easy with fiber.
Fake
Eat nothing that contains artificial flavorings, chemicals, etc.
While in a flare, your goal is to eat foods with anti-inflammatory properties.
Dr. Josh Axe reports,
One animal model also found that regular consumption of sucralose, also known as Splenda, could cause liver inflammation in mice.
If you do any sort of research on the harmful effects of fake foods, you will easily see just how much of a health problem they truly are.
Reduce or eliminate sugar
Did you know that sugar is the most potent drug? Or that the sugar addiction is real?
Harvard Health states,
Consuming too much added sugar can raise blood pressure and increase chronic inflammation, both of which are pathological pathways to heart disease.
Sugar is everywhere and in everything, so if you want my list of 192 sugar sources and alternate names you’ll find it HERE.
Be careful with carbs
But also know that you do not need to completely get rid of them.
You just need to understand which ones work for your body, and which ones do not.
Skip the coffee
I know, I know….this one is HARD.
Again, the goal is to get out of the Colitis flare as soon as possible so you can enjoy that cup of Joe again.
For now, simply try tea.
I like these three for digestion.
Don’t be afraid of fat
In fact, if you have IBD-C (constipation), up the fat intake (unless you do not have your gallbladder, then that’s a whole other issue).
No alcohol
I did my first ever Sober October in 2023. And the results were astounding.
The NIH states that,
Chronic alcohol intake leads to intestinal inflammation, including altering intestinal microbiota composition and function, increasing the permeability of the intestinal lining, and affecting the intestinal immune homeostasis.
If you want to lessen your IBD symptoms you MUST cut the alcohol. Period. End of story.
Keep your food bland
This might also mean the need for temporarily dropping spicy food as well.
No dairy
Dairy products are difficult for almost every single Gutsy girl, much less those of you who have IBD AND are in a flare state.
The physiology breaks down as such:
Lactose intolerance is a primary lactase deficiency. Lactase is the enzyme that breaks down lactose, a disaccharide, into monosaccharides glucose and galactose in the brush border of enterocytes. Lactase deficiency is the most common enzyme deficiency in the world. (source)
I have a list of 100 dairy sources and alternate names HERE.
The above are 14 key things, many more specifics relating to them can be found in my book, A Gutsy Girl’s Bible: a 21-day approach to healing the gut.
But bottom line: watch out for all the inflammatory and/or mucous-forming foods.
By the way, remember again that these “restrictions” are temporary (I mean, does your flare up last longer than 7-10 days?)! Do not make these habit.
Gut healing is not a diet, but also it might be for a short while. (+ see below my note on the gut-healing fast track.)
Food Diary
One of the BEST ways home remedies for colitis is simply to identify the foods that are causing more harm than good during any Colitis flare up is by keeping a food and lifestyle journal.
By understanding what you’re doing and eating and the outcome that’s occurring, you will be able to drastically improve your quality of life.
Get your journaling system HERE.
7 Not-Food-Related Things I Do During a Colitis Flare Up
Click HERE to save these 7 non-food-related home remedies for colitis for later.
Within these 21 things to do during a colitis flare up, I have included non-food related things because lifestyle changes are so, so important.
In fact, they might even be more important than the food list.
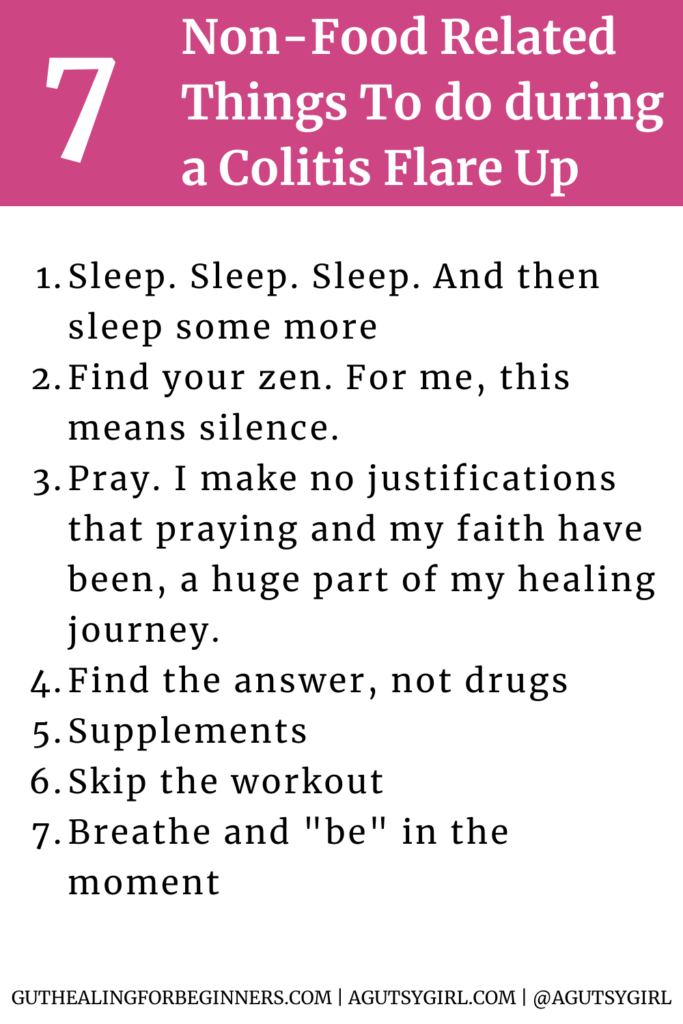
Sleep
And sleep. Then sleep some more. Now is not the time to do 2,417 things in a day. Your body needs rest, and it needs to find its deepest form of zero stress while simultaneously repairing. Whatever you have to do, make sleep happen.
Read more: Sleep and Gut Healing.
Find your zen
For me, this means silence. I find space to breathe, turn off everything and just sit. You must find your calm place while flaring.
Pray
I make no justifications that praying and my faith are and have been a huge part of my healing journey.
Jesus Christ is my true healer, but no matter what you believe, I believe you must dig deep to connect with your spiritual side during this time. Spirituality is a primary food.
Find answers, not drugs
I take LDN, confidently. I also see a holistic MD who didn’t just give me a drug, but instead provided the medical tests to find out what was actually wrong with me.
As part of your healing process, medications and antibiotics can have their place. They have been critical during my own journey.
All I’m saying is, don’t just take the drugs without understanding exactly why you’re taking it and what is truly wrong.
Supplements
I always made sure mine were on point, especially since they can be hard to remember/do on a consistent basis.
There is a laundry list of supplements that I have taken at any given moment.
I don’t know what supplements are right for you (you can find out which supplements might be best for YOU HERE), but work with your doctor and/or other medical provider to find it/them.
Know that the minimalist approach to supplements will be best in the long run.
If you are looking to save money on various foods, services, and supplements, be sure to get a copy of A Gutsy Girl’s Master Spreadsheet HERE.
Skip the workout
In the early days of healing, it didn’t matter if I was flaring and had an 8-mile run on my workout calendar. I ran anyways. Horrible, terrible, no good, very bad idea.
If I were to go back in time, I would simply do simple movements like short walks, yoga, and plain stretching.
I promise you that high intensity workouts will only have you downward spiraling more.
Breathe and “be” in the moment
We learned a few deep breathing exercises while at Nutrition School, but try breathing in for a few counts, hold for a few and then release for a few. Repeat several times.
Allow yourself to just “be” in the moment vs. thinking backward or forward.
This applies to meal times, in particular. Sit, be and eat your food in the moment, slowly. Want more on breathing? Check out: Breathe Deep.
I LIVE for helping the Gutsy community; those of you with IBS and/or IBD.
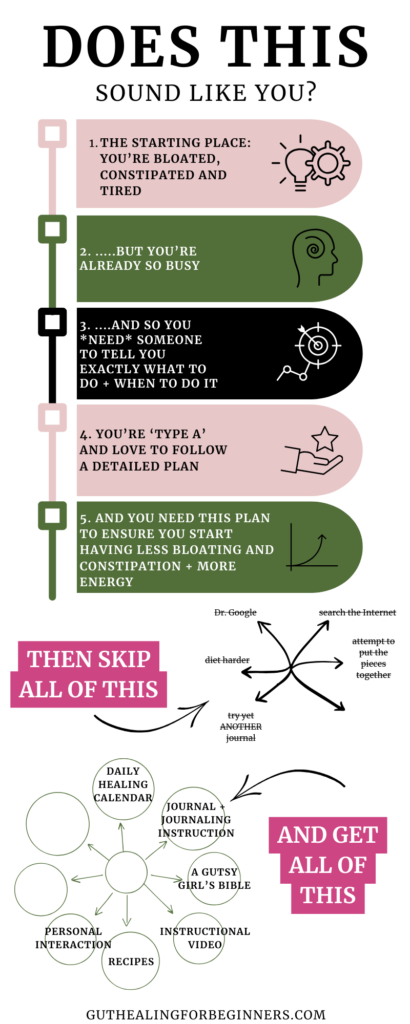
If you want my full blueprint and system for finding relief and finally getting results with a step-by-step process, consider: GUT HEALING: ELEVATED.
p.s. Once your flare ends, get yourself on the gut-healing fast track.
Our bodies are not just made up of food.
We are whole human beings, and our circumstances at any given moment might have more to do with our current well-being state when the food arrives in us vs. the actual food itself.
I have gotten a lot of help, and I have worked really hard on healing.
When it comes to food, I am reaping the benefits (i.e. eating almost everything, except gluten and dairy), feeling incredible and remaining flare-free.
My wish is for you to find the same, and in the meantime, my wish is that these tips will help you get over your next flare quickly.
If you liked this post on home remedies for colitis, you might also enjoy:
Xox,
SKH
🤰 bloating be gone! weight loss through optimal gut health for women
💃ʜᴇᴀʟ ʏᴏᴜʀ ɢᴜᴛ. ʜᴇᴀʟ ʏᴏᴜʀ ʟɪfe.
🫶🏻 founder gutbyome.com



![Psychobiotics [+ 5 other biotics to know]](https://agutsygirl.com/wp-content/uploads/2021/01/prebiotic-probiotic-featured-agutsygirl.com_.png)
I have always loved your holistic approach. And I have finally found a place where I am ready to focus on my own holistic treatment plan. It’s starting with baby steps, but I am excited about it!
Good for you! I read your post….great to hear.
Thanks for all the advice you provide on here. I honestly haven’t taken my ulcerative colitis disability seriously until just this week. I’m going through a massive flare up. It’s not pleasant. I also have a strong faith in our Lord Jesus! I appreciate that you include that in your site!
Thanks!
I have struggled with this for so many years! I’m only 20 and this is something my mother struggles with also.
I’ve only recently started worrying about the consistent damage that my ulcer is causing and I’m considering natural treatment.
I’m waiting to hear back from the lab about whether I have h.pylori which could be the cause.
Best of luck on the journey! God bless!
Good luck! I was about your age when it all began!
Try vegan! I been struggling for years. Im finally having less pain and trips to the bathroom. Less bloating! Like none! I feel better every day.
I was just diagnosed yesterday… so thank you for posting and helping a newbie out… i’m having a really really difficult time, and have shed so many tears over the past week… thank you for all you do.
Hang in there, Courtney. The journey is long and hard, but there is always hope and there are always things you can do to feel better:)
Hello I was just diagnosed with ulcerative colitis today- have you been able to do it med free? They started me on meds because it is pretty severe right now (a lot of stress I believe is the major cause of it), but I don’t want to be on the meds long term, I would love any advice or links to articles you have- I guess I should by the book!
Hi, Anna! I only take one med, which is LDN. You can look into it, but it is essentially more of an alternative medicine to help with motility. It’s given to those with autoimmune conditions primarily. Beyond that, I don’t take anything on a daily basis. I have managed all of it with diet and lifestyle. My website hosts a ton of information! Enjoy:)
Help! I have had trouble for months! Went to ER and a ct showed serious infection and Was told UC is the cause but I’m needing infection to clear for further test. I have NO IDEA what to eat! I am in so much pain and the strong antibiotics are helping it get better but my stomach is a MESS! I do not have insurance until January so that is extra stress! What do you take for pain? I was told not to tale Advil or tylonal and I tried alieve but it hurt me worse! Any and all help needed!
Hi, Crystal! I am so sorry to hear of your pain. A few things/suggestions:
1. Start with Bone Broth. Here is my free e-book on it –> http://bit.ly/skh101d55
2. For more, grab my e-book -> http://bit.ly/aggbible20
3. To work with me 1-on-1, see -> http://agutsygirl.com/start-here-2/health-coaching/
How do you know when a flare is over? If a dr has you on medication that currently has it in control, how do you know when it is safe to stop? (Other than another $300 stool sample) ????????
Hi, Sheila!
You know when a flare is over because you feel better and your “other markers” (that your doctor has been watching) improve. That said, just because you feel better does not mean you should go off your medication on your own. I rejected medications almost immediately, but had I been on them for a long time, I would not have just gone off of them without talking to my doctor. I take LDN daily, and I’d never just stop it without talking to my doctor. Hope that helps:)
I was diagnosed with UC 6 years ago. I’m just realizing that I have a flare every June that lasts all summer. I’m not sure what could be triggering it. I used to think gluten was my main trigger but I haven’t had any this year and I still had a flare. Any info on it having to do with the seasons?
Hi! I don’t. But I do know that there are seasonal allergies that crossover with different foods. Do you know if you have any allergies?
Also, with the change of seasons, sometimes we tend to eat differently. Do you start eating things in June that you don’t in the prior months?
Thank you for the information. My 16 yr old just recently got diagnosed with ulcerative colitis. It all began in July this year. She is still flaring. 🙁 The Dr. after the the scopes were done that diagnosed her problem, put her on Predisone temporarily and also started her on Mesalamine and told us she would be on this for the rest of her life! We like the more natural approach so this saddens me cuz I don’t like the idea of having her have to take synthetic drugs! I am very overwhelmed at the moment trying to help my daughter feel better. She has restarted school and is an active basketball player which is her passion. She is wore out, not sleeping at night cuz of discomfort or frequent trips to the bathroom. I hope I can learn something from your post.
All my best in healing, JoLeAnn. With some lifestyle changes, I believe she can find relief. It’s a long road, but all my very best to her!
I was diagnosed in 2014 summer with pretty severe symptoms and since then have had 7 admissions into hospital for flare ups. I must admit that since I was diagnosed at 18 years old I found it very difficult to accept the disease and thus was not taking my medication (Asacol) consistently and my diet was a mess – eating spicy food recklessly/fried food/smoking/entertaining stressful situations. (My University degree; 2014-2019 had to be mitigated a further year due to a flare up happening just as exams were about to take place- so the colitis has impacted my life so much since). Since my diagnosis I have had quite a few years of rebelling as a young adult and did not take life seriously. However with my last flare up and C-diff (explained below) and my unplanned pregnancy in November I have seen life from a different perspective.
Latest admission- (August 2018 and December 2019)
My current situation as it stands –
Due to the two recent admissions in the space of one year and the fact the doctors cannot continue to prescribe me steriods to bring the flare back into remission; the doctors have advised me to consider the next medical treatment plan to avoid having an emergency surgery. The December admission was the worst I ever had due to being diagnosed with C-Diff which I think triggered off this last flare up as my bodys immune system was weak in the post labour phase. I never felt so weak before and it really put me down the lowest I’ve ever been. I was in hospital for 2 weeks and a half and was genuinely scared I will not make it out. The doctors wanted to start me on azathioprine and inflimixb as soon as possible during my admission I am so scared about the side effects of the medication that the doctors have told me to look into while im weaning down on the seriouds and I’m wondering whether from your personal experience you could tell me if you think I should just go ahead with it or is it still not too late to change my diet and continue on the Asacol.
I cannot imagine living my life with a stoma I would of course rather take the medicine than this but I wish I could avoid it all! Theres nothing I can do about the past decisions now and I need to focus with what I have right now.
I can’t believe I never acknowledged how serious this disease is.
Thank you so much for your time in reading this. I look forward to hearing from you.
Hi Sarah –
I am 60 years old and I have had what I called tummy troubles often on over the years. When I was 18 I was diagnosed with lactose intolerant. I didn’t really pay much attention to that because it didn’t really seem to affect me that much . I had Some upper G.I. troubles but that had been under control for a while. I just found that I would have pain after eating but it would definitely go away pretty quick for sure by the next morning. I had an endoscopy and a colonoscopy about four months ago and everything was good.
But then last week I got so incredibly sick that I had to go to the doctor and then was sent to the hospital. This is very unusual for me I am very healthy and rarely get sick. I don’t really call my tummy aches getting sick because they don’t bring me down. But this one did and the doctor diagnosed me with colitis saying that it is an infection. I’m trying to figure out if what I have can turn in to ulcerative colitis or if it is a different thing. So my main question before I buy your book -is will it help me with this type of colitis which he said was an inflammation of the colon wall? I am on antibiotics for the infection and this is the fourth day since I got sick. I still have pain in my belly and I still cannot eat much without feeling terrible. I’m drinking lots of water and I have had bananas, applesauce, a few crackers, a little bit of ginger ale and some almond milk. I’m just not sure What to do at this stage to get past this flare up. So I’d like to buy your book but I was confused as to whether it is about ulcerative colitis and Crohn’s disease as opposed to what they are saying I have.
Thank you so much!