My husband was telling me a C Diff story recently. I realized how common of a term it is to me, but it might not be for everyone. Up for today is a conversation around what is C Diff?
What is C Diff
Click HERE to save this post for later.
The Center for Disease Control (CDC) estimates that C. difficile infects approximately half a million Americans each year.
Ironically, the first time I ever heard of and started researching C Diff was when I watched this show called One Mississippi. Did you ever see it?
Here I was, fascinated by this woman, Tig Notaro, who faced ugly, traumatic life forces.
One of those things being C. Diff. The TV show portrayed it as her in the bathroom 24/7, frail, and weak.
Curiosity had me exploring.
In simplest terms, Clostridium difficile or C. Diff for short, is an intestinal infection (which colonizes in the large intestine) that can spread through spores and cause diarrhea.
Harvard shared a great pictorial explanation of this “bad bacteria.”
Although doctors are working hard to control intestinal infections caused by the bug commonly known as C. diff, the problem is rapidly becoming more common, more serious, and harder to treat.
But why?
How Do You Get C. Diff?
In the past, it was commonly thought that only older patients in hospitals and/or at long-term care facilities who had taken a course of antibiotics were susceptible to C. Diff.
This is no longer the thinking because of how the bacteria spreads.
According to Mayo Clinic,
C. difficile bacteria are found throughout the environment — in soil, air, water, human and animal feces, and food products, such as processed meats. A small number of healthy people naturally carry the bacteria in their large intestines and don’t have ill effects from the infection.
Spores from C. difficile bacteria are passed in feces and spread to food, surfaces and objects when people who are infected don’t wash their hands thoroughly. These spores can persist in a room for weeks or months. If you touch a surface contaminated with C. difficile spores, you may then unknowingly swallow the bacteria.
Once established, C. difficile can produce toxins that attack the lining of the intestine. The toxins destroy cells, produce patches (plaques) of inflammatory cells and decaying cellular debris inside the colon, and cause watery diarrhea.
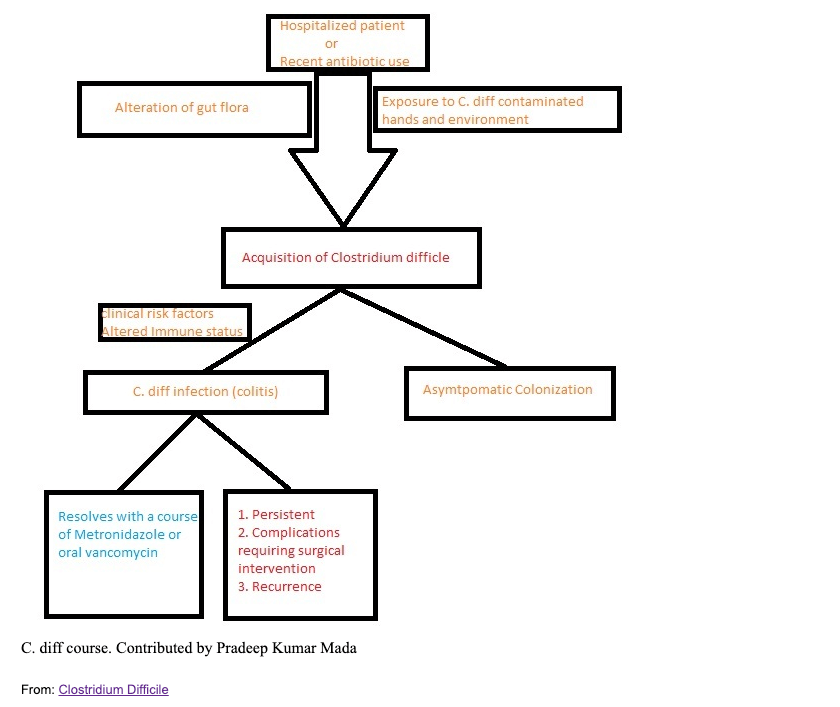
Even still, there are some common risk factors:
- Antibiotics
- Fluoroquinolones
- Cephalosporins
- Penicillins
- Clindamycin
- Proton pump inhibitors, which is used to reduce stomach acid
- Age (more than 80% of C. diff deaths happen among those 65 and older)
- Complicated medical care and extended stays in healthcare settings, especially hospitals and nursing homes
- A weakened immune system
- Previous infection with C. diff or known exposure to the germs
- Chemotherapy
- Chronic renal disease
- Chronic liver disease
- Malnutrition
What are C Diff Symptoms and Complications?
Symptoms range from general, less frequent diarrhea, to life-threatening inflammation of the colon.
They tend to start within one month of taking an antibiotic, though usually it shows up within just a few days of starting the antibiotic.
Initial Symptoms Can Include
- Diarrhea including loose, watery stools (poop) or frequent bowel movements for several days
- Fever
- Stomach tenderness or pain
- Loss of appetite
- Nausea
Advanced Symptoms Can Include
- Watery diarrhea 10 to 15 times a day
- Abdominal cramping and pain, which may be severe
- Rapid heart rate
- Fever
- Blood or pus in the stool
- Nausea
- Dehydration
- Loss of appetite
- Weight loss
- Swollen abdomen
- Kidney failure
- Increased white blood cell count
Complications
The complications of C. Diff range from common to rare.
Common complications include: dehydration, colitis, and severe diarrhea.
The more rare complications include: serious intestinal conditions, such as toxic megacolon, sepsis (the body’s extreme response to an infection), and even death.
How Do Doctor’s Test for C. Diff?
If your doctor suspects C. Diff, they will do a test to appropriately diagnose you.
The CDC says these are the most common tests.
C Diff Test
1] Molecular tests:
These tests test for the gene encoding toxin B, are same-day tests that are highly sensitive and specific for the presence of a toxin-producing C. diff organism.
Molecular assays can be positive for C. diff in individuals who are asymptomatic.
2] Antigen detection for C. diff:
These are rapid tests (<1 hour) that detect the presence of C. diff antigen.
Because results of antigen testing alone are nonspecific, antigen assays have been employed in combination with tests for toxin detection, PCR, or toxigenic culture in two-step testing algorithms.
3] Toxin testing for C.diff:
Tissue culture cytotoxicity assay detects toxin B only.
This assay requires technical expertise to perform, is costly, and requires 24 to 48 hours for a final result.
4] Stool culture for C. diff:
This test is the most sensitive test available.
It is the one most often associated with false-positive results due to the presence of nontoxigenic C. diff strains.
The stool culture has a relatively slow turnaround time (i.e. results available in 48 to 96 hours), making them less clinically useful overall.
What is the C Diff Treatment?
When you first started reading this post you may have wondered, “Well, what was the context of the C. Diff story your husband told you?”
The context included one possible treatment. That treatment is the fecal transplant.
While this is still not the most common form of treatment, it is proving successful for many.
What is a Fecal Transplant?
A fecal transplant is exactly what it sounds like: transferring one person’s (healthy) poop into another person’s colon.
They are not used as the first line of defense. Typically an FT (fecal transplant) is considered when the individual is not responding to the common antibiotics (listed below).
According to Infection Control Today,
Unlike antibiotics, which are destructive by definition, fecal transplants or microbial replacement therapies, repopulate the gut with a diverse group of microbes that may block the C. diff’s spore from germinating and propagating disease via its toxins. Transplants have several delivery methods, including enemas, capsules and direct instillation, to replace the diverse flora that maintain health and improve metabolism.
Th fecal transplant is not currently FDA-approved, though there have been many success stories from the procedure.
The challenge is ensuring that the “healthy” fecal matter is truly healthy.
This includes very careful stool screening prior to the procedure. To date, there isn’t a universal screening standard.
In addition to the fecal transplant, there are other, more common, current treatments.
Common C. Diff Treatments
- Antibiotics (yes, more antibiotics!). Common ones for C. Diff include oral vancomycin or fidaxomicin. Extended regimens, lasting several weeks, have been used successfully to treat recurrences. Vancomycin enemas and intravenous metronidazole, another antibiotic, are also used in severe cases.
- Colon resection or a colon-sparing procedure. This procedure is for patients with severe C. Diff who are not responding to other therapies.
Reason #1,004 for Building a Strong Microbiome
Various women in the Gutsy community have gotten C. Diff.
Questions around the topic are coming up frequently.
This is why I chose to write about it and share as much as I could today.
For the Gutsy community, some of the risk factors are simply unavoidable.
Just look at some of your Gutsy stories featured, and you’ll see frequent hospital stays.
There is no shame in that. And it’s okay if, while you’re in the hospital, you take one of those antibiotics. I mean, maybe it saved your life?
C. Diff is the result of an unfortunate reaction, though.
But the facts about it remain: C. Diff is a type of bacteria that can produce toxins that attack the lining of your intestines.
So while you can’t control a lot of it, you can focus – every single day – on building the strongest microbiome possible.
Remember, the bacteria colonizes in the large intestine.
The goal is to have more “good bacteria” crowd out the “bad” in order to fight the C. Diff.
And how does that happen? Check out How to Achieve Optimal Microbiome Diversity HERE.
If you enjoyed this post, you might also like:
Sources: HERE, HERE, HERE, HERE
Xox,
SKH
🤰 bloating be gone! weight loss through optimal gut health for women
💃ʜᴇᴀʟ ʏᴏᴜʀ ɢᴜᴛ. ʜᴇᴀʟ ʏᴏᴜʀ ʟɪfe.
🫶🏻 founder gutbyome.com


![Rosacea vs Seborrheic Dermatitis [+ other gut-skin issues]: Podcast Episode 48](https://agutsygirl.com/wp-content/uploads/2022/08/ep-48-rosacea-vs-seborrheic-dermatitis-podcast-featured-agutsygirl.com_.png)