Today I get to share with you my interview with Onegevity co-founder Dr. Joel Dudley.
One of the other 752 reasons I love working for you at A Gutsy Girl, is that I get to dig deep into the people and stories behind the products and brands out there desperately wanting to help us.
Many times, these people have a story similar to us. They know and understand where we came from, what we’ve been through, and (maybe most importantly) what we actually need.
And oftentimes, I also get the chance to speak to highly educated and intelligent individuals who know something about the gut and overall health that I haven’t studied in depth.
Dr. Joel Dudley
Dr. Joel Dudley, co-founder of Onegevity, would be one of these people.
He is also a Crohn’s patient.
His career’s work is focused on developing and applying methods to integrate the digital universe of information to build better predictive models of disease, drug response, and scientific wellness.
In 2016 Joel Dudley played an integral role in invalidating Theranos’ technology. In which, Dr. Dudley published the first scientifically rigorous review of the technology in a study in the Journal of Clinical Investigation.
In addition, Dr. Dudley is the Executive Vice President for Precision Health at Mount Sinai and is the Director of the Institute for Next Generation Healthcare at the Icahn School of Medicine at Mount Sinai.
His work has been featured in the Wall Street Journal, Scientific American, and other popular media outlets, and he was named in 2014 as one of the 100 most creative people in business by Fast Company magazines.
I’m really excited to share more about our conversation to help you understand more about the company and microbiome in general.
Interview with Onegevity Co-Founder Dr. Joel Dudley
Click HERE to save this post for later.
Crohn’s Disease
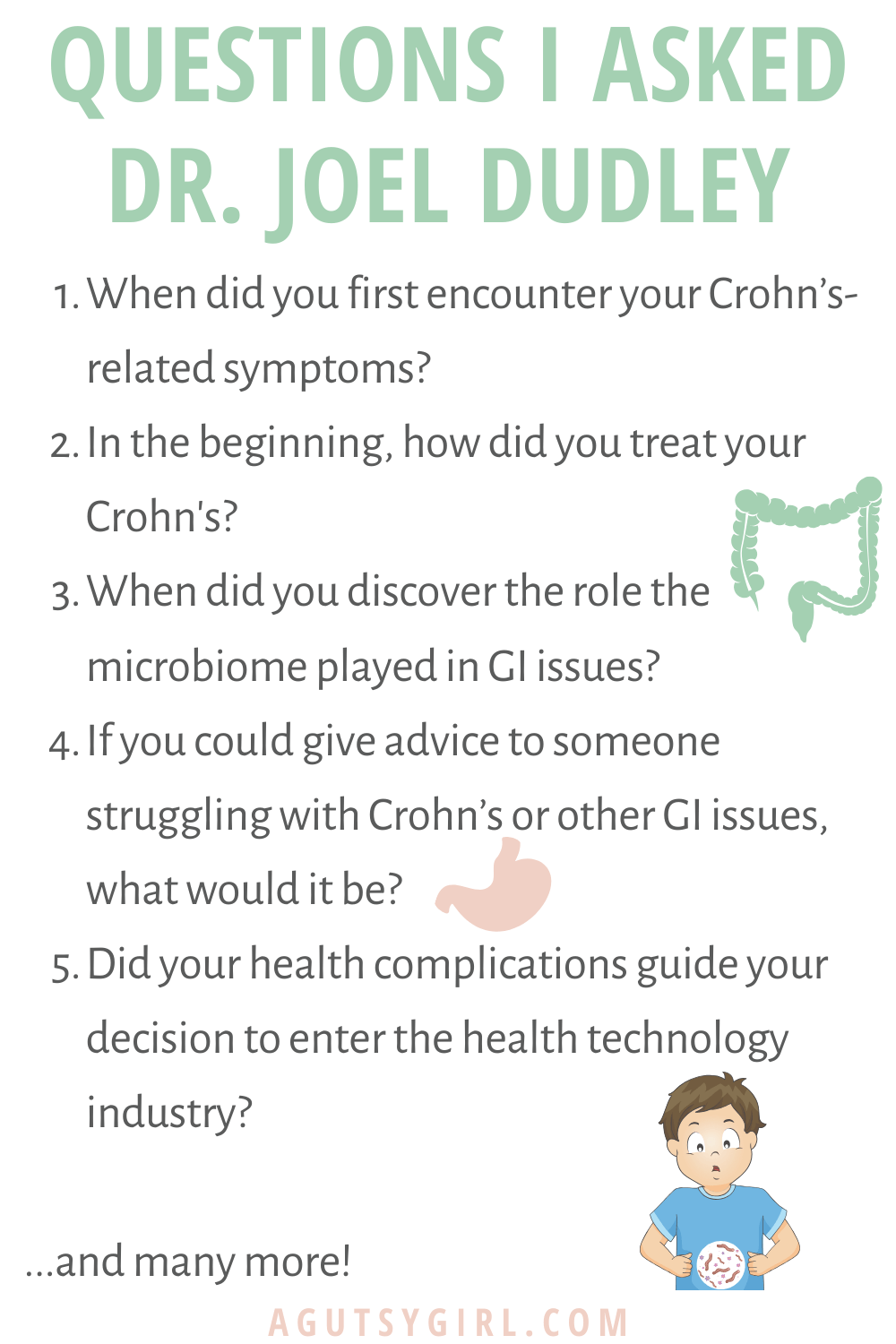
When did you first encounter your Crohn’s-related symptoms?
DJD: I think it’s one of those things where once you went to get diagnosed, you can rewind the tape and go back your entire life and realize, ‘Oh, that’s what that was, you know?” I can recall symptoms going back to when I was young that were clearly tied to Crohn’s in terms to having pain in my stomach and things like that.
However, I didn’t get diagnosed until I was 30, but my sister had it at a younger age. In fact, I have a sister and a half sister that both have it. So it’s a very interesting genetic experiment in my family.
What lead you to get help for the Crohn’s?
DJD: About 12 years ago I went to the emergency room. I had actually just started grad school and went in with this unbelievable pain in my gut. I thought it was a burst appendix and in fact, that’s what the ER department thought.
They did a CT scan and saw pretty classic Crohn’s, and started asking my family history. It’s pretty funny the cognitive dissonance you can have because even though I had two sisters with Crohn’s disease, I wasn’t thinking that I had Crohn’s. I think your brain partially doesn’t want to think that, you know?
So I was diagnosed immediately. At that point it was quite severe.
The type of Crohn’s I have has fibrosis and stenosing characteristics, which means that the pipe basically gets scar tissue built up over time due to inflammation deep in the tissues.
And the inflammation, the patterns of constant inflammation, create a sick scarred tissue. By that point, I basically only had about a pencil’s width of room in the terminal ilium, which is where your small intestine connects to your large intestine; a classic site of Crohn’s.
In the beginning, how did you treat it?
DJD: I went to Kaiser Permanente in California. I met with a young, GI doc who was actually more advanced in her thinking. She talked through options; there’s drugs you try before surgery. So she wanted me to start with drugs, first.
It’s actually interesting cause the pharmacogenomics is how you use genetic testing to see how you react to drugs. She tested me for this gene called TPMT. TPMT dictates how you respond to Azathioprine drugs, which 6-mercaptopurine which is a treatment for Crohn’s, a thiopurine drug. So I actually had a mutation that meant I was a slow metabolizer of 6-mercaptopurine.
From that standpoint, it was interesting to have an innovative physician do some additional genetic testing. But she did prescribe 6-MP, which is a drug that’s used for chemo and other things. If you look at the side effects, they are pretty severe. Like many drugs to treat autoimmune disease they basically ravage your immune system and increase your risk for leukemia, lymphoma, and all sorts of other things.
Systemic or Localized?
So that got me down the road of thinking, you know, why do I need a systemic toxic compound to address this disease that is actually quite localized, in terms of just effecting part of my gut? And that got me looking pretty heavily for alternative ways to treat it.
I started with a very strict regimen of following the specific carbohydrate diet, which I’d come across in my Internet searches. And that actually worked quite well for me, if you’re very strict. The reason I liked it was because it had some scientific rationale for it which is often hard to find.
AGG side note: HERE is more on the SCD Diet.
One thing I’ll point out is I remember when I told my GI doctor I was going to try a diet based intervention and wasn’t going to take the mercaptopurine. She smiled at me and said, “I’ll see you back in two weeks to cut your intestines out.” Of course, I didn’t go back to the ER for many, many, many, many, many years after that.
Crohn’s and the Microbiome
Did your health complications guide your decision to enter the health technology industry?
DJD: Yeah, for sure. To be clear, I’ve always been interested in biology and genetics, and so I was headed that way anyway.
And in fact, my mom found a paper I wrote in sixth grade, or a little article I wrote in sixth grade that said I wanted to be a geneticists. So I always had that interest, but how I did the research, and then obviously starting Onegevity and other things is all very directly tied to my perspective being a patient.
When did you discover the role the microbiome played in GI issues?
DJD: It’s Interesting. It never seemed to me when I studied it, the genetics and other things of it, that Crohn’s was similar to the other autoimmune diseases. It definitely overlaps with other autoimmune diseases but something was different about is the genetics and microbiology of Crohn’s and ulcerative colitis.
And that told me something else was going on.
The simple traditional model of an autoimmune disease, of course, is you get auto antibodies, let’s say against the some healthy tissue cell surface receptor, right. And your antibody, your auto antibodies incorrectly detect your normal cells as pathogens and you start to damage your own tissue.
But the biology was a little different for Crohn’s. And then of course we know that the gut is full of bacteria.
We just didn’t know what the heck they were doing, or who was supposed to be there and not be there.
Technology
There was the sequencing technology evolving to the point where we could measure the microbiome in a holistic way, meaning measuring all the bugs that are in there at once. And then there was the genetics of Crohn’s and ulcerative colitis being revealed by genetic studies being a bit different than other autoimmune diseases. Of course there’s overlaps too. It all made me realize that there must be something else that’s going on in terms of the environmental interaction, the food and how it could be mediated with the microbiome.
So then obviously researchers were starting to study the microbiome and in particular IBD and gut health. However, that hadn’t been translated into personal use.
And I was actually part of some efforts. I was on a paper when I was a grad student, but that was the first ever. It’s kind of silly to think about it now, but it was the first ever use of a personal genome for a clinical workup.
It’s funny to think you could get a huge paper published just by looking at one person’s genome back then. And then, I wrote a book: Exploring Personal Genomics.
I was kind of an early adopter in the personal genetics space. So then I got very interested in looking at my own microbiome. The only options you had at the time back then were Ubiome, which is now out of business.
Onegevity: the Company
Metagenome Sequencing
DJD: The first technology that was used for this (by UBiome) was called 16S ribosomal RNA sequencing, which gives you sort of a low resolution. You have your whole genome, but it gives you a broad view of your whole genome.
So the first thing I wanted to do was get a snapshot of where I was so I could build up a profile of how my microbiome was changing over time. Initially I was just interested in getting a snapshot and figuring out where I was. I didn’t expect to find any smoking gun-bacteria, and then see the effects of dietary changes and things like that.
But the technology got better.
Metagenome Sequencing
So at Onegevity, we do shotgun metagenome sequencing, which is far higher resolution than 16S is.
The analogy I always use is that 16S is like black and white TV from the 1950s. And metagenomics is like 4K ultra HD TV.
It’s that big of a difference in information and resolution. There’s rarely a single gene. The one thing I knew from personal genetics is there’s rarely just one gene that’s going to explain everything that’s going on.
It’s usually a combination of things, which is why we needed whole microbiome sequencing. It’s really about the ecosystem and not about any sort of particular bug, although some bugs have more influence than others. But I’m a data guy and I want data to drive all my decisions. So that was my initial interest.
Co-Founder Dr. Chris Mason
DJD: I met Chris when I moved to New York and became a professor at Mount Sinai school of medicine. We met Chris through that network of genomics people in New York, and we both happened to be from the same state; born and raised in Wisconsin. We connected over that and other things.
I was connected to his research and he had a really cool study where he did microbiome sequencing of the whole New York city subway system that is kicking off. Really cool stuff.
There’s sort of a minority view, unfortunately, in biology at least. So we were naturally attracted to each other because we’re much more of these data-driven, systems-thinking, sort of researchers.
Shared Interests
Chris was pioneering microbiome research, but Chris also had an interest. I think another area we share a belief that Chris calls it, genome Liberty or something. It’s the idea that a patient should have access to more information.
There’s obviously schools of thought where patients should not be given access to lots of information because people think they don’t know how to handle it. I think Chris and I are on the other end of the spectrum where we both have always believed that individuals should have access to as much information as possible to make decisions about their health.
For years we had discussed the idea that we should really do something about this. Can we start a company, and what can we do?
And eventually we found an opportunity to start Onegevity together to work towards that. There are a number of other reasons why we decided we wanted to start Onegevity based on the research.
Who Will Fund the Studies?
I’ll just give one example. One thing you realize when you are in academic research and NIH funded research is that basically nobody is doing it.
So it was this chicken and egg thing where the doctors always say, “Well, there’s no evidence for diet-based interventions. And then what you say is, “Well, who the hell is going to fund that?”
Right? Nobody would find that study.
Nobody meaning the NIH and pharma won’t fund that research, and they are the two people that fund most of the research in the world.
So in our country, if they’re not going to fund it then who the heck is going to fund it? The answer is no one. And that just didn’t seem satisfactory to me.
I’m not against pharmacological intervention. In fact, I know and work with pharma companies and they do some really important work. But the traditional models were never ever going to fund rigorous scientific studies for food based or nutrition based interventions.
Chris and I are quantitative and highly heavily scientific oriented people and we want that evidence base. So we realized that we could start a company that would directly interface with consumers and build that rigorous evidence base as a means to fund that.
Clinical people tend to figure about how can we control and focus on a single variable. But single variable almost never explains anything in biology or health. For example, a single gene or a single protein almost rarely explains anything that’s going on completely.
Food is a mixture of things with a multitude of interactions with the microbiome. So in the traditional biological and clinical research model, that’s just very complicated and people just don’t want to deal with it because it’s hard. And so again, you need statistics and data science and other things to be able to really tease that apart.
And that just happens to be what Chris and I are experts in.
His Crohn’s Advice
Now that you know so much about the microbiome and GI health, what are some initial thoughts?
DJD: There’s some super interesting things in my own personal microbiome data. One thing that happens when you have Crohn’s and you flare up consistently is that you get antibiotics as part of the treatment.
I have serial microbiome measurements for myself over a long period of time.
Microbiome
The state of your microbiome is like a multidimensional space with mixtures of various microbes. And that’s like a topographic map. And what I was able to see in my data is I basically fell off into a cliff or into a pit. Meaning, for whatever reason, almost all of my probiotic bacteria were killed by antibiotics, and they haven’t come back.
The microbiome bacteria in your gut occupies various niches right in your intestinal lumen and the brush border cells of your small intestines. And there’s all these different gaps and spaces and, when you take antibiotics some bacteria die, but there’s other bacteria that don’t and they move in.
These bacteria don’t like to leave once they have a spot, just like squatting, right? They’re like, “Ooh, this is a nice new occupied apartment. Someone just left the door open here. I’m going to just move in and take this.”
So you can take antibiotics or probiotics like lactobacillus and things like that. Then they’ll come back and try to get back into their apartment, but the locks are changed and they can’t get back in.
Destroyed Microbiome
What happened to my microbiome is that over the course of repeated antibiotic treatments, I basically lost a lot of my key probiotic species and they were not coming back.
In effect, when I started to take probiotics, I would get sick because sometimes the probiotics can try to get back in and they can have interactions with the bacteria that are the dysbiosis.
And then that can cause inflammation and things like that. To be honest, probably what I need personally is to fully reset things. I’m not advocating everybody go out and do this, but for me personally a reset probably means to consider a fecal transplant at this point, just because my microbiome is so far gone.
What lifestyle changes did you make?
DJD: Other than just trying to stay active and all that good general stuff, I would say in general that I’m always worried about inflammation.
Inflammation is a root to so many diseases. I mean, it’s unbelievable. Inflammation is super complex just to be clear. It’s not like there’s inflammation of a single dimension in your body and if it goes up, it’s bad. There are different forms of inflammation, and some of it is highly beneficial; some of it is damaging. Some inflammation is beneficial in the short term but then damaging in the long term. (I just want to say as a public service announcement is inflammation is both good and bad.)
Inflammation
It’s just the right type of inflammation and the right kind at the right time. You don’t want to get rid of it completely. But obviously chronic inflammation is bad. That’s something I track.
Sleep manages chronic inflammation, inflammatory markers effected by sleep, effected by exercise.
I personally like to do heavy weight training because I have a short attention span and I get bored running, things like that. But I prefer weight training at least being a part of your regimen rather than not just because inflammation is actually key to muscle tissue remodeling. (And too much cardio can definitely be highly pro-inflammatory for sure.)
What happens when you lift weights and you actually damage your tissue, inflammatory genes like IL-6 and other genes that people might associate with disease are actually important.
Your body induces a pro-inflammatory state in your muscles that actually is the instigator of tissue remodeling and adding muscle, etc like that. If you have this regular cycle of damaging and repairing your tissues in this way it can actually help sort of keep your inflammatory response healthy.
Hormesis
There’s a concept called hormesis, which effectively means “what doesn’t kill you, makes you stronger”. It’s clear from a lot of things that induce longevity is that minor insults or moderate damage to your body and healthy doses basically increases resilience.
I’ll give you example; high-heat sauna therapy or even a resveratrol or some of these other sort of longevity associated compounds. They’re actually mild cellular toxins. And it’s really the mechanism of resilience that they introduce into the body by sort of mildly damaging the cells.
But it’s again, what doesn’t kill you, makes you stronger.
For Crohn’s, and in your situation, which PREbiotics do you like best?
DJD: One thing I noticed, there’s a couple of interesting Keystone species in the microbiome. You have to remember the microbiome is like an ecosystem and to think that you can just introduce a single bacteria and it’s going to fix everything is a very overly simplistic way to think about it. If you introduce a new bacteria, other bacteria are gonna respond to that and you’re really setting off a wave of changes in the microbiome that effects the whole ecosystem.
Akkermansia muciniphilla
However, there are some species of bacteria that have undo sort of influence over many other bacteria. Those are sort of like generals of your microbiome and one of them would be Akkermansia muciniphilla which is a super interesting microbe, one that you actually cannot get in probiotics formal because it’s very unstable outside of your gut.
It’s very hard to package up as a nutritional supplement for example. But what it does is it kind of grows actually. Your gut is constantly shedding a mucus or producing mucus to protect itself from everything in your gut.
So what Akkermansia does is it actually eats this mucous that’s produced by our gut, which is like a long chain kind of polysaccharide type, like most mucus. And then what it does is the byproducts of that mucus produces metabolites and then other bacteria eat that, those byproducts of our commodities.
So in some way, Akkermansia is like the mama bird in the nest who’s eating, like owls, that regurgitate food. It’s like an analogy, that Akkermansia is sort of like eating food and then regurgitating it. It’s not really regurgitating, but it’s feeding many other bacteria.
And plantains!
So there are some bacteria that have undue influence over many other bacteria. I actually had zero detectable levels of Akkermansia left in my entire microbiome due to antibiotics. But I was able to build it back up through, through eating lots of prebiotics that seem to feed it. And there’s beans and plantains and things like that that can target Akkermansia. So personally that has had beneficial effects on my symptoms.
If you could give advice to someone struggling with Crohn’s or other GI issues, what would it be?
DJD: I would say you do want a diagnosis. Don’t self diagnose. For a number of reasons.
Diagnosis
One, IBS and then Crohn’s and ulcerative colitis are all different biologically. Of course they share things, but they have different fundamental underlying biology, which requires different fundamental approaches to how you address them.
If you self diagnose with the wrong thing, you could be doing the wrong interventions. What is also important about getting the official diagnosis is really understanding what type of disease you have.
Even with an IBD diagnosis, there’s a whole spectrum. You can have IBD or Crohn’s at the terminal ilium, diffuse Crohn’s, there’s microscopic colitis, etc. There’s a whole spectrum and there are probably many, many more. We don’t know about split subtypes of disease.
You should also know how far along you are.
I could take, let’s say a probiotic, lactobacillus or some bifido or some fast growing bacteria, and because I had no normal immune function in that wasteland of disease tissue, it actually would cause a massive intestinal overgrowth like rapidly. The reason is because basically it’s just like scorched earth that doesn’t function normally anymore, you know?
So, even though I might’ve read a study that said it was beneficial in some people with Crohn’s, you’d have to say, “Well, what stage of disease was present, and things like that.”
That’s my PSA on getting an accurate diagnosis.
Prevention
At some point it’s just so far gone that you basically just have a chunk of dead tissue, just plumbing. I think it’s important to point out because I am the biggest proponent of natural ways to manage the disease. But at some point, there’s not much you’re going to be able to do with natural approaches and you’re just going to have to cut out the bad plumbing. What’s the phrase?
A ounce of prevention is worth a pound of cure.
So that’s why it’s important to intervene early. This is obviously biased because this is why we created Onegevity. But you don’t have to take a microbiome test. You could do symptom tracking and things like that, but just try to understand a little bit about how you test the hypothesis and try to test things in a controlled way.
The problem is people try to change a thousand different things at once. And then it’s hard to know the thing that’s working. So then there’s a whole range of things, right?
SKH Note
This part of our conversation was one of my favorites. When he talked about diagnosis and prevention, I mentioned,
It goes along with what I say all the time. Think about these three pillars when it comes to digestive health. The first is diagnosis, the second is food / diet, and the third is lifestyle.
He completely agreed with these pillars.
And by the way, if you are interested in taking the Onegevity Health GutBio test, click HERE. Then, use code AGUTSYGIRL20 at checkout for $20 off.
If you liked this post, you might also enjoy:
- Intro to Microbiome Testing with Onegevity
- What I Really Think About Workouts and Gut Healing
- A Gutsy Girl’s Three Pillars
Disclosure: This post is a paid partnership with Onegevity. All opinions stated here are 100% my own. I appreciate your support, as this compensation helps with expenses to keep this blog up and running, and for me to continue sharing all that I can with you. For my full disclaimer and disclosure click HERE. Thank you for your support!
Xox,
SKH
🤰 bloating be gone! weight loss through optimal gut health for women
💃ʜᴇᴀʟ ʏᴏᴜʀ ɢᴜᴛ. ʜᴇᴀʟ ʏᴏᴜʀ ʟɪfe.
🫶🏻 founder gutbyome.com