Is this your first time here? Cats out of the bag. I have Colitis, namely Proctitis so I wanted to share more about Colitis and Proctitis.
You may have heard of IBS before, yes? Colitis is not IBS. Colitis is an inflammatory disease, better known as IBD.
If you search around on IBS and IBD, you will find a lot of information on both; theories, some good stuff, but also plenty of garbage.
What is the difference between IBS and IBD?
IBS and IBD are not the same things. IBD is characterized by disease; IBS by syndrome.
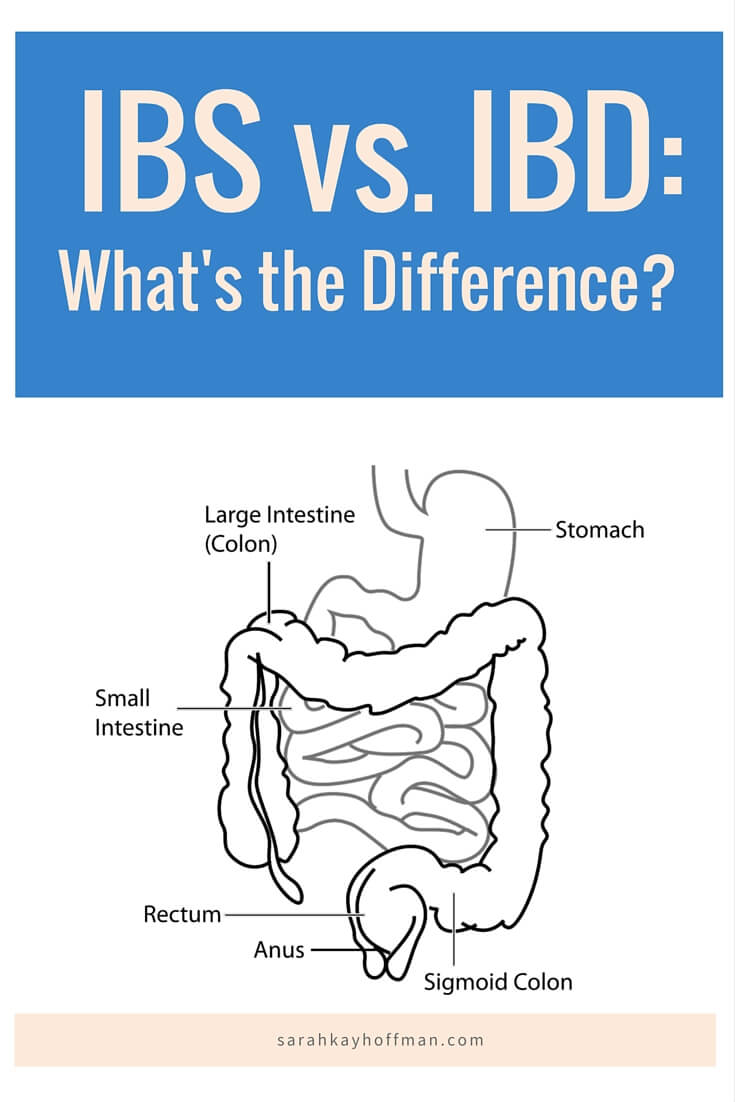
In simplest terms, IBS is the term doctors who have done all due diligence on testing give for a disorder that affects the motility (muscle contractions) of the colon. IBS is less serious because it’s a set of complications which are (less) non-specific than direct disease inflammation.
BUT….that is not to discount IBS, the pain and the agony people that have it go through.
Colitis and Proctitis
Click HERE to save this post for later.
What is Colitis?
Colitis, specifically ulcerative colitis, is
a chronic (ongoing) disease of the colon, or large intestine. The disease is marked by inflammation and ulceration of the colon mucosa, or innermost lining. Tiny open sores, or ulcers, form on the surface of the lining, where they bleed and produce pus and mucus.
People with colitis can have any of the following symptoms: abdominal pain, blood in stool, change in bowels, constipation, fever, weight loss, fatigue and more.
Colitis is classified as many different things, and depending on what classification you fall under, your symptoms likely vary. This is the reason why people think when I say I have colitis it’s the typical colitis….it’s typically not what they think. I have ulcerative proctitis, but there is also: proctosigmoiditis, left-sided colitis, pancolitis and fulminant colitis.
What is Proctitis?
Proctitis is what I have been “diagnosed” with. Why do I use the ” ” around diagnosed? Because it’s been several years since, and I had only had that one opinion, from one GI and via one colonoscopy. Part of me believes it. Part is skeptical.
When ulcerative colitis affects only the lowest part of the colon — the rectum — it is called ulcerative proctitis.
Does this sound gross? Too bad. Deal with it – you’re already here:)
I am skeptical, mostly, because of how The Mayo Clinic defines it. Those were not my symptoms, and I have never felt like I have the mildest form.
Updated in 2019: It’s nowhere to be found!
Colitis and Proctitis
According to the Crohn’s & Colitis Foundation of America,
Colitis is marked by an abnormal response by the body’s immune system. The immune system is composed of various cells and proteins. Normally, these protect the body from infection. In people with IBD, however, the immune system reacts inappropriately. Mistaking food, bacteria, and other materials in the intestine for foreign or invading substances, it launches an attack. In the process, the body sends white blood cells into the lining of the intestines, where they produce chronic inflammation. These cells then generate harmful products that ultimately lead to ulcerations and bowel injury. When this happens, the patient experiences the symptoms of IBD.
There are many theories, thoughts, and ideas that lie around colitis and (for me) proctitis in general.
If there is one thing I’ve learned after the past several years of battling it, it’s that having a form of IBS or IBD is not the end of the world. I’ve also learned that there is so much to learn.
Your doctor is a critical component in helping you find out if it’s IBS or IBD. Furthermore, they are equipped to do all necessary testing to determine what you actually have (Celiac? Colitis? What kind?) and to what severity. And how long it takes to heal depends on your ability to appropriately (not self) diagnose. Click HERE to learn more about that.

What I Have Learned
But I have also learned that most doctors don’t believe there is anything you are or are not eating that could help or hurt you even more (unless you have Celiac Disease).
And this is tragic.
The digestive system sure is a large place with a mammoth effect on all the body’s systems to believe that what we put in it has no effect….don’t you think?
It’s why I made it my mission to help women worldwide heal with food and lifestyle.
I am living proof that it can be done, and I have helped thousands of women realize a better way, too.
Digest it.
Xox,
SKH
🤰 bloating be gone! weight loss through optimal gut health for women
💃ʜᴇᴀʟ ʏᴏᴜʀ ɢᴜᴛ. ʜᴇᴀʟ ʏᴏᴜʀ ʟɪfe.
🫶🏻 founder gutbyome.com


![Stomach Bloating After Exercise [Ways to Get Rid of It]](https://agutsygirl.com/wp-content/uploads/2014/01/stomach-bloat-exercise-featured.png)



great post! I think I suffer with a form of IBS which was triggered by a bad bout of food poisoning. I used to never have problems and now sometimes I do with constipation, bloating, sharp abdominal pains, etc. It’s no fun at all! This is very informative!
Hi Heather! Yes, it’s all usually “triggered” by something. I’m so sorry to hear of your struggles, but you are not along & there are so many things you can do to feel awesomesauce:) Let me know if I can ever help!
we digest the same
The doctors tend to also diagnose people with IBS when they can’t figure out what is wrong with you. I have been told I have IBS by one doctor who was short with me and told me there was nothing one could really do about it. And then I was told by another doctor that I could have a case of IBS on top of something else but they are not sure what… beside my tortuous colon and possibly colonic inertia. What did the doctors do for you to diagnose you with what you have?
Yes…that is why it’s a “syndrome.” I had a colonoscopy and endoscopy to diagnose.
See I have had both of those.. no go.. thats when they found my lower esophagus was weak and that my colon was tortuous. They couldn’t even finish my colonoscopy on account that my colon was so long and loopy 🙁 so I ended up having a barium enema xray to make sure there were no blockages anywhere they couldn’t get through
Hi, I have been diognosed with Proctitis, Do you have any information on what causes it? Also, are you taking anything to help it. I have taken Mezaline suppositories but every time I stop the Proctitic is back within a couple of weeks
Hi Candie! Here is some more info: http://bit.ly/skhwip No, I do not take anything to help with it, and I have been healed for a couple years now. I used to take suppositories. They only made me worse. I manage everything with food and lifestyle. Feel free to check out my story & the services I provide. Reach out anytime…I’m always listening 🙂 sarahkayhoffman@agutsygirl.com
I have Crohn’s disease. Lost most of my colon back in 1990. Recently I had a rectal dilation and Dr. was pushing Humira on me. After reading up on Humira I opted for no drugs and have been following a more plant based diet. Stopped most dairy. I feel SO much better. I do still have issues with the rectum but I am trying to heal myself my way. I was also looking into IIN. Haven’t made the leap yet but I’m getting there.
You are amazing, Vickie! I sent you a follow up email. Please let m know how I can support you or if there are additional IBD topics you’d love for me to blog about:)
I was diagnosed with proctitis last June and am currently in the middle of a rather severe flare. Have you ever been able to get it under control? Currently I’m on canasa and cortenemas, my tailbone hurts so bad that I cannot sit down. Being a stay at ahome mom (on break from college) with a 3 year old – resting is out of the question. It’s tough to keep a positive perpective when your on the toilet at least every hour. Have an apointment next week and am worried the GI will put me on oral steroids as well. I really don’t eat much dairy – is there any foods that seem to trigger for anyone else?
Hi Sandy! I have proctitis, and I have been hoping to meet another female with it as well. I was on canasa for a bit, but it made me worse. It was at that point that I made the personal decision to go OFF of it and change my entire lifestyle, beginning with an elimination diet and heal myself. It worked. I understand how hard it is to be positive when you feel so horrible. Yes, they will likely put you on more meds next week if you are in a lot of misery. You might have an extreme case and truly need meds. But remember, medication is simply masking your symptoms. It’s not solving the problem. There could be so many different food and/or lifestyle factors that are contributing. Read these 2 posts:
1. Is Stress Causing My Digestive Distress? http://bit.ly/agugscdd
2. The Elimination Diet http://bit.ly/agugted
I would love to work with you once I open my business. Feel free to reach out anytime: sarahkay.hoffman@agutsygirl.com
ALL MY BEST!!
Last Friday the GI put me on Flagyl and by Sunday morning the pain was gone – so it must have been an infection too? Today the pain is starting to be noticeable again – still taking the Flagyl, Cortenema & Canasa. I have an appointment tomorrow and am a bit anxious for it – being my second flare and constant bleeding – it’s hard to judge for myself if this is severe or not. I really feel that the Cortenemas have made things worse; from the first one I used. The Canasa kicked my first flare (May 2011 – August 2011) but there was hardly any bleeding & no pain – just nuisance. LOL.
Glad you mention the diet changes – when I first was sent to the GI they put me on a strict diet until my scopes. My symptoms were nearly gone when they scoped me & of course the procedure re-started the flare. Just two weeks on that diet & it was immensly better. Perhaps I need to take that route. Thanks for the links I’ll check them out once I get my 3 year old in bed.
Reach out to me anytime, Sandy!