Have you ever wondered, “What is the best diet for IBS flare up mode?”
I’m giving you the goods today with the hopes that you are able to not only find some instant relief, but also to help you understand how you might navigate that IBS diagnosis moving forward.
Best Diet for IBS Flare Up (Episode 103 with Dr. Sara DeFrancesco)
Click HERE to save this information on the best diet for IBS flare up for later.

Episode 103: Show notes

Episode 103 on the ‘A Gutsy Girl’ podcast: Best Diet for IBS Flare Up with Dr. Sara DeFrancesco.
Today’s episode focuses on all thing IBS and what to do when a flare-up occurs.
Subscribe Today:
Apple Podcasts | Spotify | iHeart Radio | RSS
In this Episode we cover:
- Who is Dr. Sara DeFrancesco?
- What exactly does IBS consist of? And what are some common IBS symptoms?
- When a client comes to Dr. DeFrancesco with an IBS flare-up, where does she start?
- What does Dr. Sara think are some common trigger foods for an IBS attack?
- If someone is having IBS flare up, what might their bowel movements be like?
- In the case of an IBS flare, what are lifestyle changes one could make immediately?
- Does Dr. Sara think IBS has to be a chronic condition? If not, what are some tools or tactics she likes to employ to get her clients out of that vicious cycle?
- Are there any dietary supplements Dr. Sara thinks are good for IBS flares that IBS sufferers might consider?
Links & Resources Mentioned in this Episode:
- Follow Dr. Sara on Instagram
- Dr. Sara’s website (I have also added her to the ‘Practitioner Referrals’ tab via the Master Gutsy Resource Spreadsheet)
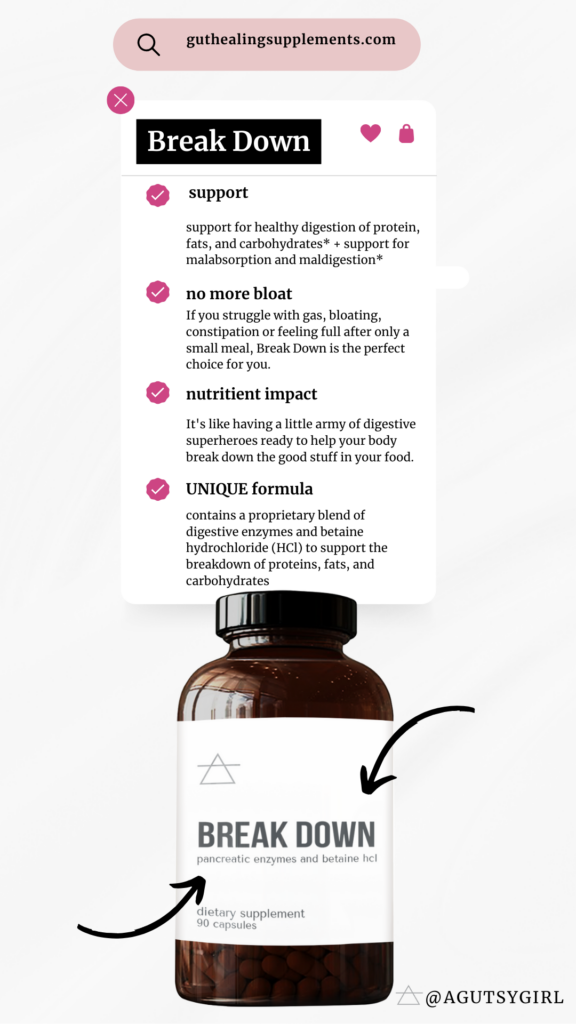
- Break Down – the digestive enzyme from A Gutsy Girl’s line (code: PODCAST will save you 15% at checkout)
- A Gutsy Girl’s journal
Episode Images
More about the A Gutsy Girl podcast
A Gutsy Girl is the podcast that teaches, preaches, and celebrates healing the gut and living a happier, healthier life.
More episodes you might enjoy:
IBS Overview
We have covered IBS (irritable bowel syndrome) in great detail over the years on A Gutsy Girl, but in case you’re just entering the gut healing and/or gut health world for the very first time, I wanted to give a brief overview.
First, what exactly is IBS?
IBS is known as “spastic colon,” and since it’s a syndrome it’s just a set or range of symptoms that may fall into the defining category, Irritable Bowel Syndrome.
IBS, unlike IBD (inflammatory bowel disease), does not cause tissue inflammation. In other words, if you were to be ‘scoped,’ doctors would not find tissue inflammation, scarring, etc. from IBS alone.
(However, if you were scoped and did have a form of IBD, you would discover that. It would not be a pleasant finding, but critical.)
It is a condition that sort of acts as an umbrella for many other symptoms and is a diagnosis that’s typically given when “all else has been ruled out.”
(Do make note, though, that typically everything else hasn’t truly been ruled out since IBS is mostly just a symptom of something deeper going on.)
IBS Symptoms
The symptoms of IBS are varied from person-to-person.
Everyone is different, namely because some have the IBS-C (constipation) version and others have the IBS-D (diarrhea) version while others have the alternating version which includes both constipation and diarrhea.
But in general, IBS sufferers experience things like:
- abdominal pain
- constipation
- diarrhea
- both constipation and diarrhea, alternating
- gas
- bloating and/or distention (not the same things)
- mucus in stool
- nausea
What Causes IBS?
To be clear, no one truly knows what causes IBS.
Here are some theories:
- Disturbance in the gut-brain axis.
- Irregular colon motility patterns. In other words, how fast food moves through you is either too fast or too slow.
Let me be very clear, I think the statement “it’s just IBS” is BS.
I believe that when given the diagnosis “IBS,” there is always more to the story.
Said IBS doesn’t get any better, usually gets worse, because the root cause is not determined.
In fact, HERE are 7 roots causes of IBS.
IBS Flare-Up
If you’re here today, the chances that you have been told you already have IBS are pretty high.
And in that case, you were wanting to know,
What exactly should I do during an IBS attack?
Here are the specific things Dr. Sara discusses on Episode 103.
1. Get Quick Relief
Focus here for 7 – 14 days. This is the critical time for calming your digestive system. Her ways for going about this:
- Ensure you are breaking down your food at each meal. Take a digestive enzyme. THIS is precisely why we have Break Down, the super-high quality digestive enzyme for the Gutsy community.
- Identify your trigger foods immediately. Do this with a food and lifestyle journal so that you know which specific foods are contributing to the flare-up symptoms:
- Did you eat steak or other red meat and immediately have problems? Consider low stomach acid.
- Are you having a difficult time digesting vegetables like sweet potatoes, cruciferous vegetables, and other plant foods? Consider low digestive enzymes and / or a bacterial overgrowth like small intestine bacterial overgrowth (SIBO).
- What happens when you eat fatty foods? This could be a sign of poor bile flow.
Then…
2. Remove Trigger Foods
If you are journaling in the correct way and keeping track of the IBS triggers by way of food, you can remove those foods for a short period of time.
Common Food Triggers for IBS
Here are some common triggers for IBS patients in general:
- Dairy products, including but not limited to; ice cream, cheese, any and all milk products
- Gluten
- Foods high in high fructose corn syrup
- Sugars and artificial sweeteners
- Alcohol; alcoholic drinks
- Coffee and caffeine in general (soft drinks)
- High-FODMAP foods (FODMAP stands for Fermentable Oligosaccharides, Disaccharides, Monosaccharides and Polyols)
Dr. Sara also mentions that food triggers are specific to the individual, too, based on specific conditions. i.e. Acid reflux or gastritis = acidic and/or spicy foods.
A special note on fiber
Fiber is always going to be debatable when it comes to IBS and/or any conversation regarding the IBS diet and digestive symptoms.
Because I don’t believe there is one specific way for approaching fiber, I’m empowering you to do the research and then make sure you’re keeping track in your journal.
Here are some articles I have written in the past to help you navigate:
3. What to do about Bowel Movements?
One of the hardest parts of IBS flare ups is the unpredictability of bowel movements.
For some, there is too much – aka, diarrhea and for others, not enough – aka constipation.
The goal is to have a complete, formed bowel movement every single day.
And what does that mean + look like? Check out the Bristol Stool Chart information HERE.
Dr. Sara advises to do what you have to do to arrive here.
4. Lifestyle Changes
During an IBS flare up, the last thing you think could help might be the thing you actually need.
And this, of course, is any specific lifestyle change.
Dr. Sara offers these suggestions:
- Spend time in nature.
- Stimulate the vagus nerve.
- Do something you love; something that is fun for you.
Additionally, I’ll add:
- Get small amounts of physical activity (this could be as simple as a walk in nature!)
- Sleep, sleep, and then sleep some more.
- Spend time in prayer, meditation, or something similar. Even practicing various breathing techniques can truly help!
5. Supplements
In my opinion, part of both diet and lifestyle includes supplementation.
Here are some Dr. Sara particularly called out for an IBS flare-up:
- Digestive enzymes
- Specific fiber, as tolerated (ex. chia seeds, raspberries, psyllium husk)
- Magnesium citrate for constipation
- Probiotics
- Peppermint tea or ginger tea (herbal teas in general)
IBS; Chronic Condition
Dr. Sara and I discuss the idea of IBS as a chronic condition some.
The good news is that it doesn’t HAVE TO be a chronic condition.
It becomes one when healthcare professionals continue telling their patients things like,
It’s all on you
And….
This is a lifelong condition.
But we must dig deeper.
IBS is a matter of WHAT not WHY.
And if you’re experiencing IBS flare up after flare up, then consider that your IBS diagnosis is not what you’ve been told.
There are many health conditions to consider, and the sooner you can address your severe symptoms and arrive at the correct diagnosis, the faster you’ll actually heal.
It is my hope that you only have to read information about “what to do during an IBS attack” once.
This should not be a commonplace stay for you.
Wrap-Up
As always, a huge goal for this show is to connect with even more people. Feel free to send an email to our team at podcast@agutsygirl.com. We want to hear questions, comments, show ideas, etc.
Did you enjoy this episode? Please drop a comment below or leave a review on Apple Podcasts.
Bio: Dr. Sara DeFrancesco
Dr. Sara is a Naturopathic Doctor, Functional Medicine Practitioner, and expert in digestion, mood & brain health, and autoimmunity who healed her own IBS, anxiety, and panic attacks and put her autoimmunity into remission.
Using holistic medicine, specialty testing, neuroscience, and mind-body tools, Dr. Sara creates personalized plans to remove obstacles to healing, correct imbalances, and allow dysfunctional systems to heal.
If you liked this podcast episode on the best diet for IBS flare up, you might also enjoy:
Xox,
SKH
🤰 bloating be gone! weight loss through optimal gut health for women
💃ʜᴇᴀʟ ʏᴏᴜʀ ɢᴜᴛ. ʜᴇᴀʟ ʏᴏᴜʀ ʟɪfe.
🫶🏻 founder gutbyome.com