What is Diverticulitis, and how could I have been diagnosed with it?
New, and very common questions I’m getting.
What is Diverticulitis
Click HERE to save this post for later.
Diverticulitis is inflammation or infection in small pouches called diverticula.
Diverticula range from pea-size to much larger.
They are formed by increased pressure from gas, waste, or liquid on weakened spots of the intestinal walls, and are most commonly found in the lower portion of the large intestine (the sigmoid colon).
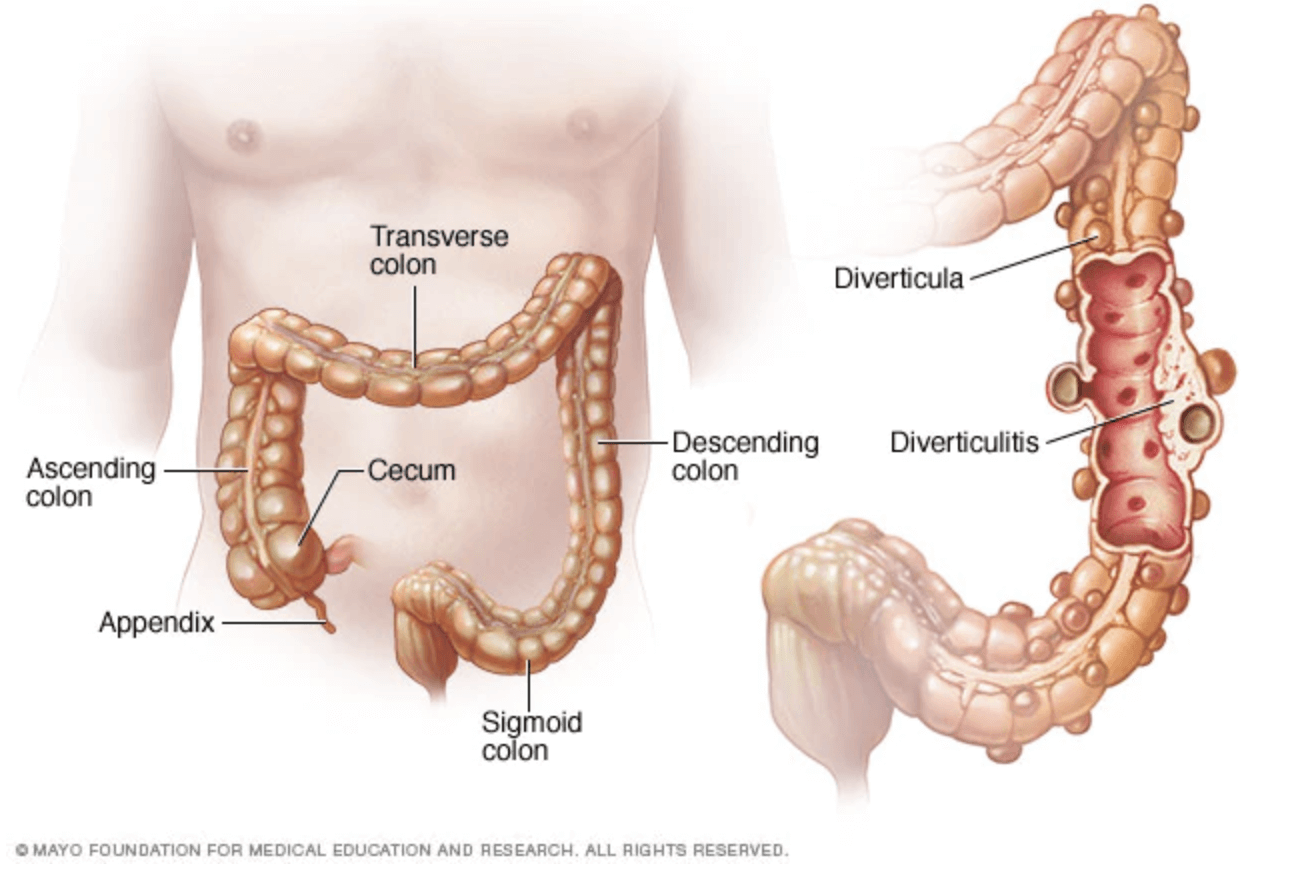
Image credit: Mayo Foundation
According to Harvard Health,
Diverticula tend to develop where the muscles are weakest, at the places where penetrating vessels cross through the muscles. And in Western societies, the great majority of diverticula develop where the colon is narrowest, in the sigmoid.
Diverticulosis vs. Diverticulitis
According to the NIH,
Diverticulosis is one of the most common gastrointestinal conditions affecting the general population in the Western world. It is estimated that over 2.5 million people are affected by diverticular disease in the United States.
Diverticulosis is when the small pouches, diverticula, form.
Diverticulitis is when one or more of them become infected and inflamed.
Thus, not everyone who has diverticulosis will necessarily have it develop into diverticulitis.
Diverticulitis Signs and Symptoms
Click HERE to save these for later.
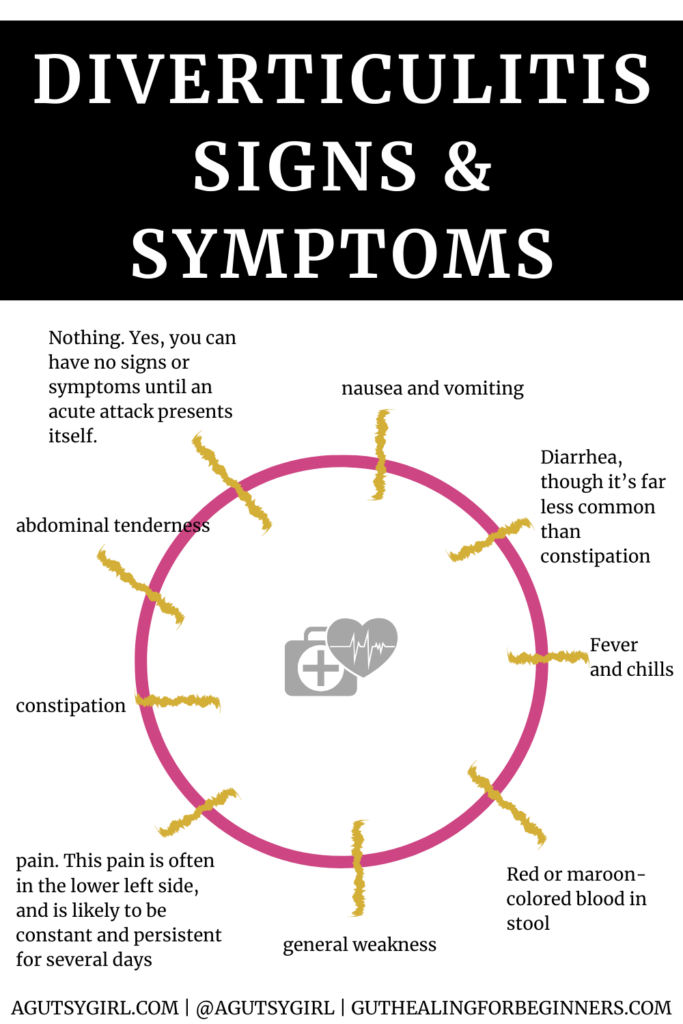
Like everything else gut related, the signs and symptoms can be different for everyone.
These are some of the common ones for people who have diverticulitis:
- Nothing. Yes, you can have no signs or symptoms until an acute attack presents itself.
- Pain. This pain is often in the lower left side, and is likely to be constant and persistent for several days.
- Nausea and vomiting
- Fever and chills
- Abdominal tenderness
- Constipation
- Diarrhea, though it’s far less common than constipation
- Red or maroon-colored blood in stool
- General weakness
Symptom tracking is easy with my gut healing journaling SYSTEM, Ahara Dinacharya.
Causes and Risk Factors of Diverticulitis
Harvard Health says this about Diverticulosis,
The principal factor is diet, especially the refinement of carbohydrates, which has deprived the typical American diet of much of its fiber content. Diverticulosis is a disease of Western civilization.
Here are the common causes and risk factors for diverticulosis (which, as mentioned, many times turns to diverticulitis):
- Age
- Lack of dietary fiber
- Obesity
- Smoking
- Lack of exercise
- High animal-fat diet
- Certain medications including steroids, opioids and nonsteroidal anti-inflammatory drugs, such as ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve).
Diverticulitis Diagnosis
The way diverticulitis is generally diagnosed is reactively, meaning, once someone is having an acute attack, they will go in out of intense pain and it’s discovered.
- A physical examination where the doctor may be able to feel tenderness in the abdomen.
- A CBC (complete blood count), which could indicate infection with high white blood cell counts.
- CT Scan. Medical equipment can be hugely expensive (for example CT scanners for sale are very expensive machines) too so it’s worth considering just how much medical practices have to spend on such equipment.
- Colonoscopy
The first three are typically done immediately; the fourth, as it involves much more, some time after.
But also, if you have had regular-ish and/or a recent Colonoscopy, they would have likely seen it. Remember, do not be afraid of the Colonoscopy. It can be life-saving. HERE are some (30 to be exact) tips to help get you through.
Treating Diverticulitis
For the short term, because it’s a bacterial infection, antibiotics are almost always prescribed. These range from Augmentin to Flagyl and Cipro, depending on the person and their circumstances.
For severe cases, IV antibiotics may be administered at the hospital.
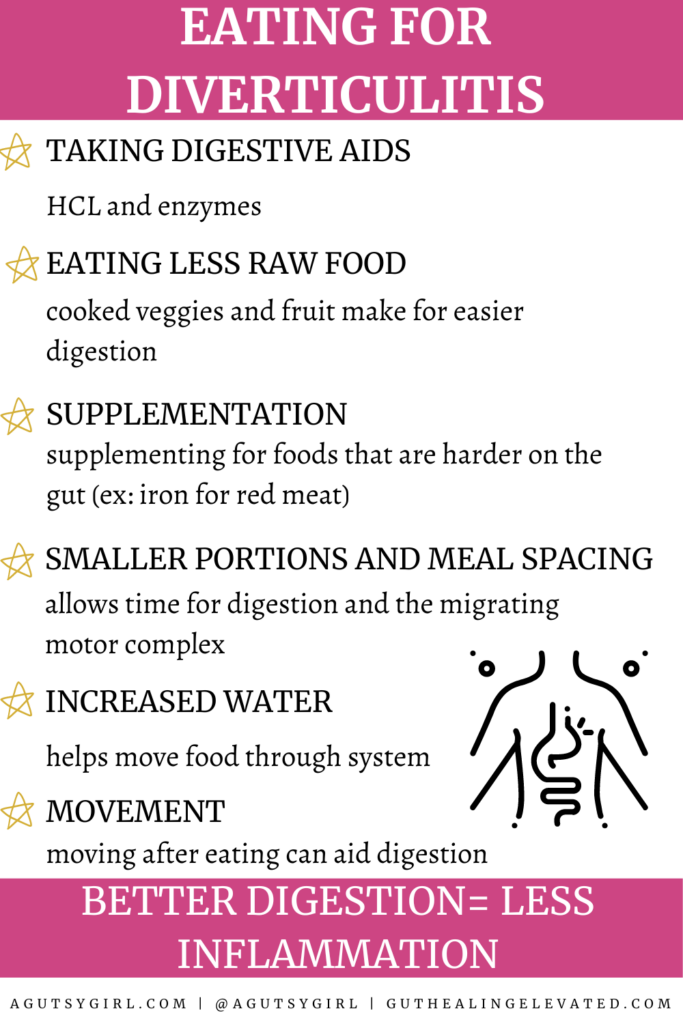
After that, sticking to a diet of clear liquids for a few days, then gradually adding soft solids and moving to a more normal diet over a week or two. Vegetable and/or bone broth anyone?
Because it tends to reoccur, prevention then is key.
Foods to Avoid if You Have Diverticulitis
While May Clinic is no longer saying you don’t have to avoid any foods with Diverticulitis, there are the ones they have said should be avoided in the past:
- nuts
- seeds
- popcorn
The theory is that they get stuck in the pockets (diverticula) and cause the inflammation (or an acute attack).
However, since two of the main causes are a lack of fiber and high animal-fat consumption, it can be generalized that, once an acute attack has ended, avoid foods with little fiber/no nutritional value and high animal-fat content.
What to Eat During a Diverticulitis Acute Attack
I will always tell it exactly like it is.
Many who lean more holistic will tell you “always eat whole, unprocessed foods…..squeaky clean – more fiber is better, etc.”
But I won’t.
Because while I’ve never had diverticulosis or diverticulitis, I know that healing the gut can and does require something different than keeping the gut healthy and well.
Being in a reactive state is not the same as when you get to be in a proactive state.
During an acute attack, you need to respond reactively. So if it were me, acting reactively, with a diverticulitis acute attack, I would:
- Consume only soothing, clear liquids for at least 1-3 days. This would include non-caffeinated teas, broth (both vegetable and bone), homemade jello, and maybe even homemade popsicles.
- Once I was certain the absolute worst of it was over, I’d introduce easy to digest foods. And no, this still does not include 25+ grams of fiber per day. Common things I’d choose would be lean meat that is tender (likely even slow-cooked; slow and go), eggs, well-cooked vegetables de-skinned and de-seeded (I talk a lot about this in A Gutsy Girl’s Bible: a 21-day approach to healing the gut), some plant-based fats like olive and coconut oil and/or avocado, white rice, and of course everything still from the first few days. I would stay here until I was feeling at least 80-90%, and then, I would begin adding in more fiber daily.
- Take any and all antibiotics the doctor prescribed. Depending on the severity, likely no questions asked.
- Consider a probiotic. “In one prospective open trial by Fric and Zarovral, Escherichia coli strain Nissle 1917 was administered to 15 patients with uncomplicated diverticular disease. These patients had longer periods of remission and improved abdominal symptoms after receiving probiotic compared to before treatment.” (source)
Simple, Not Easy
Looks so easy. It’s not. And also, if you’re going through an acute diverticulitis attack but have never tired these basic few steps, what do you have to lose?
Nothing.
What I have found in the past 10+ years of researching, studying, and living all things gut and digestive issues is that no one believes this stuff until they are forced to try a new way.
If today is that day for you, take it.
You never know where the road might lead.
If you liked this post, you might also enjoy:
- The Beginner’s Guide to Digestive Health Testing
- Home Remedies for Diverticulitis {+ Episode 64 with Joanna Fowler}
- Foods that Cause Bloating During Period (Episode 82: gut health and menstrual cycle)
Questions?
Xox,
SKH
🤰 bloating be gone! weight loss through optimal gut health for women
💃ʜᴇᴀʟ ʏᴏᴜʀ ɢᴜᴛ. ʜᴇᴀʟ ʏᴏᴜʀ ʟɪfe.
🫶🏻 founder gutbyome.com







I have recently been searching foe information online w search engines and found this to be the best read yet. Thank you so much.
Thank you! Do you have Diverticulitis?
Hi and thank you for the interesting points!.
I was diagnosed last month, after spending over a week and a half in hospital I was released. Personally I felt better than ever until a fruit salad landed me back with all the symptoms again. Currently, I am under my G.P’s care and hoping to have the energy levels back for Christmas.
I have had diverticulitis for many years. I had the lower portion of my colon removed several years ago. I have an attack every few months and it is so painful. I take steroids for severe asthma daily. I have so much empathy for anyone who suffers with this problem. Thanks for the info
Thank you for sharing. Xox
Today I was diagnosed with diverticulitis and after reading this I feel so much better not so worried and more informed thank you so very much
Thank you very much for all this information. I am currently in the hospital being treated for this condition (first time being diagnosed with this.) I will need to make a lot of changes so that I don’t end up with a flare up.
Please note that CIPRO and that entire class of Floroquinolones are extremely dangerous. The FDA has issued a black box warning in 2017/18.It can have deadly consequences. Also apparently newer research didn’t find a need to limit diet,although I have had too during the first few days just to feel safer. I’m exploring a gluten free diet which is a pain,but after living with several flares and such,I think it’s worth a try…so far so good
Thank you so much for all the info . Best I’ve seen so far! Being the first time diagnosed yesterday this will be very helpful. Also, I’m a visual person so actually seeing those great photos of what my “innerds” look like right now is awesome!
Thank you so much, Barbara! All my very best.
Thank you for the article . You worded it so nice for such a painful issue . I have had diverticulitis many times over the past few years but just in the last three months it gotten much worse and more frequent flare ups . Thanks for the tips and would love read more about guy health from you . Thanks !
Thank you so kindly, Rachel! Thinking of you….
I’ve read several articles recently, since I was just diagnosed. I thought I was doing everything right. I eat healthy…very little red meat (fat) and lots of fruits and vegetables., no junk food, chips etc. Turns out, MY culprit was most likely 800mg Motrin for arthritis/back/hip pain. I didn’t know it has messed with my GI tract in a recurring way. Thank you!
You’re welcome. I hope you start healing 🙂
Thank you for this article! I was just in the ER with my first attach. It has rocked my world because I have worked hard on healing my gut for the last 4 years. I follow the AIP diet-fiber, moderate exercise, drink lots of water- until 9 weeks of quarantine. I went lax on the diet ate a kiwi, lots of fruit smoothies. I’ve not been exercising as much. My mind is having a hard time wrapping around this diagnosis. All i know is I never want that pain again……NEVER!
Thank you again for this article.
Thank you for sharing, Paula. Thinking of you…
I understand you, Paula. I just was diagnosed last week after my first flare-up. I am on a soft diet right now and feel just a tinge of pain every so often. I, like you, don’t EVER want to feel that pain again. It was horrible. I told the doctor it felt like labor pains that constantly come and go. When you are not having a baby this is not fun at all. I’m still trying to wrap my head around it all and researching daily. There are so many conflicting articles and videos. I DO NOT WANT THE PAIN is all.
My diagnosis is severe diverticuliteous. Has never flared up before. One of my concerns is the nausea is in the upper position of my stomach not in lower position. Once I take a nausea pill it goes away. Is this normal?
I was diagnosed with diverticulitis several days ago. My MD instructed me to take antibiotics prescribed and eat a high fiber diet. I’ve eaten nothing for 7 days and have been almost totally anorexic since the pain started. Thankfully I had enough sense to know that was not good advice. Too bad my doctor didn’t read this article! Thanks for your advice.
Hang in there, Liz. Thinking of you.
I knew I had diverticulosis and had had a few mild attacks through the years. Just had a major attack. Spent 3 days in the hospital. Had a perforation.
I just lost 30lbs and now I’m supposed to follow this diet. Just makes me so sad. I may talk to the nutritionist at our local hospital and ask her to help me come up with a plan. I refuse to gain it all back. I have arthritis and fibromyalgia and a low carb diet was so good for me. My pain level was way down.